This popped up yesterday.
Here is the link to the blog that has the comment.
http://aushealthit.blogspot.com.au/2014/12/aushealthit-poll-number-250-results.html
Anonymous said...
"This simply shows how blinded your readers are and how out of touch you lot are from what is really going on. NEHTA has probably the best technical leadership it could possibly hope for. This year will see SMD solved, PCEHR purring along and NASH and HI refactored to meet changing demands. The only downside is that this blog will no longer have a role
December 29, 2014 8:14 PM
When I first read this I wondered if it was serious - and felt it needed to be treated as a parody. Re-reading it came to me just how silly it actually is - and really confirms that someone is wandering somewhere in a very large swamp of confusion - or is a good comedian!
Look at the internal in-consistency?
The best technical leadership leads to NASH and HI still (after many years) wandering in the wilderness.
The best technical leadership leads to SMD still hardly being used compared with the private sector offerings of Healthlink, Argus, Medical Objects and so on.
The best technical leadership leads to a PCEHR ‘humming along’. Of course it is as there are no users to interfere with the virtual silence of the ‘humming’ made by all that money flowing out the door.
I would really like the blog to not need to exist but with commentators like the above, who just might believe what they write (although I very much doubt it!) I feel a need to shine a little light into some very dark, very useless and very expensive places.
Ï suspect it is fair to say the readership of this blog are rather better informed than our friend cited above....
Happy New Year to all who are holding onto their sanity!
David.
Note: Comment 3 from Bernard is also spot on!
D.
This blog is totally independent, unpaid and has only three major objectives.
The first is to inform readers of news and happenings in the e-Health domain, both here in Australia and world-wide.
The second is to provide commentary on e-Health in Australia and to foster improvement where I can.
The third is to encourage discussion of the matters raised in the blog so hopefully readers can get a balanced view of what is really happening and what successes are being achieved.
Tuesday, December 30, 2014
Sunday, December 28, 2014
AusHealthIT Poll Number 250 – Results – 28th December, 2014.
Here are the results of the poll.
Holiday Poll: Will The Government Deliver A Working, Easy to Use, Safe, Clinically Useful And Widely Adopted PCEHR In 2015?
For Sure 3% (4)Maybe 6% (10)
Neutral 1% (1)
Probably Not 29% (45)
No Way 60% (93)
I Have No Idea 1% (1)
Total votes: 154
A pretty clear response with the large majority believing there is little chance of a useful PCEHR being delivered in 2015.
Good to see a clear outcome.
Again, many, many thanks to all those that voted!
David.
Tuesday, December 23, 2014
A Challenge: What Are the Five Things Australia Needs To Do To Develop A Transformative, Cost-Effective e-Health System?
In welcoming the appointment of the new Federal Health Minister the Consumer Health Forum raised 5 key points it wanted to see actioned.
The second point was as follows:
“2. Commit to eHealth: The revolutionary changes (and cost savings) possible in health care through the introduction of a robust, consumer-centred eHealth system cannot be underestimated. Funding commitments must be made beyond 2014-15 to realise the potential of this system.”
In a brief response to this point I suggested that I was keen to have some of what the authors were inhaling on the basis that I believed to imagine that such was possible, if the present directions and approaches were continued and funded, was rather unrealistic.
Here is the full link:
Hardly surprisingly I was challenged to say what I would do in five points - so here goes.
Action One:
Recognise that there are two distinct clients for e-Health systems and services and that their needs are not by any means the same - meaning that different systems are required for each. The professional clients (doctors, nurses, allied health etc.) need systems that enhance their clinical capabilities, improve record keeping and facilitate their secure sharing of clinical information to improve patient care and safety.
The consumers need systems to allow them to record their own information while at the same time having access to, ideally, the live clinical systems so they can better engage with and understand and contribute to their care.
It is obvious the present PCEHR does neither of these things well.
Action Two:
We need to recognise we don’t need a single monolithic System but that we need an e-Health ecosystem where health information flows efficiently, accurately, securely and privately between appropriately credentialed actors within the health system and to and from consumers.
Action Three:
We need an updated National E-Health Strategy that consults all stakeholders properly and provides the governance, leadership, strategic technical, standards and managerial pathways to actually achieve the goals cited by the CHF for this domain. We then need the Strategy properly funded and led - as did not happen with the 2008 version.
Action Four:
Before anything more is done or spent actually undertake a proper in depth peer-reviewed evaluation of what e-Health in all its guises has achieved in Australia and what has been achieved in the rest of the world that might be applicable to Australia. This research should inform what comes next.
Action Five:
We need to understand that no-where in the world has a transition to e-Health been easy, uncomplicated, pain free or without missteps. As we increasingly realise, getting this right is a very considerable and some might suggest near impossible challenge that takes lots of time, lots of money and dedication - as well as quality leadership and governance for success. E-Health is not something for generalist bureaucrats and technicians to have repeated goes at and repeatedly fail at!
I could ramble on for ever on this - but it what is said above is taken seriously, actioned and funded there is hope. If not then the next 20 years will be the same as the past 20!
David.
David.
Sunday, December 21, 2014
I Would Award The Hon. Peter Dutton M.P. An F- For His Performance In E-Health!
The story:
He gets into office as Health Minister - kicks off a six week review of the PCEHR - releases it 6 months later and is yet to actually to provide a Government response 8 months later!
In passing leaves industry and Standards setting out in the cold and fails to properly evaluate what has been delivered for the $1.0 Billion or so!
F- is generous - but as low as the scale goes.
As for the co-payment debacle - his change of job says it all!
God help all those poor asylum seekers and refugees.
Here is a profile of the new Health Minister:
http://patricklion.files.wordpress.com/2014/05/leyfeat.pdf
David.
He gets into office as Health Minister - kicks off a six week review of the PCEHR - releases it 6 months later and is yet to actually to provide a Government response 8 months later!
In passing leaves industry and Standards setting out in the cold and fails to properly evaluate what has been delivered for the $1.0 Billion or so!
F- is generous - but as low as the scale goes.
As for the co-payment debacle - his change of job says it all!
God help all those poor asylum seekers and refugees.
Here is a profile of the new Health Minister:
http://patricklion.files.wordpress.com/2014/05/leyfeat.pdf
David.
Has Anyone Else Noticed Just How Political The Political Leadership Of General Practice Is? The Good - They Have Now Actually Listened And Toughened Up Big Time!
This week we have seen the most amazing set of political turn-arounds I have seen in quite a while.
Let’s start with the AMA.
When the Medicare Co-Payment Plan B was announced the view was that the plan was a ‘mixed bag’. After a week and a few (the most ever) angry e-mails from those in the trenches we get:
“Last week I wrote to you outlining the details of the Government's latest co-payment proposal and asked for your feedback to help inform our ongoing advocacy.
Many members took the opportunity to respond, and I really value the constructive input you have provided.
As I said in my email, the AMA does not oppose co-payments for people with adequate means.
The AMA does not support measures that take billions of dollars out of general practice, undermine the viability of individual practices, and ultimately disadvantage our patients.
I write to make it clear to you that the AMA is strongly opposed to all three measures in the Government’s package that attack general practice, these being:
· the $5 cut to Medicare patient rebates for general patients;
· the non-indexation of rebates until July 2018; and
· the introduction of time-based changes to level B consultations.
This is a triple blow that will hit general practice like a wrecking ball. The AMA will do all it can to stop these destructive changes.”
Full letter to Members here:
Suddenly the mixed bag is a wrecking ball!
The AMA in WA is even more contrite:
AMA WA president Michael Gannon agrees to oppose GP co-payment
- December 19, 2014 11:30PM
- Perth Now
THE WA president of the Australian Medical Association has changed his mind on the federal government’s modified GP co-payment scheme after speaking to members.
Michael Gannon last week called for MPs to support the policy to charge patients an optional $5 co-payment that would be determined by doctors — putting him at odds with the national office.
But after speaking to GPs this week, Dr Gannon said he now believed the policy would have a major negative effect on the provision of health services in Australia.
Lots more here:
With the RACGP we also saw a rather ‘limp wristed’ response. A week later we get:
General practice unfairly targeted in revised co-payment model: RACGP membership
18 December 2014
Following extensive consultation and dialogue with its membership, the Royal Australian College of General Practitioners (RACGP) has strengthened its position on the Government’s revised co-payment model announced last week and is calling for an immediate halt to any measure that jeopardises general practice services.
The RACGP is astounded and disappointed that the Government has targeted general practice in its pursuit to ‘save’ the health dollar by proposing a model that will equate to higher out-of-pocket costs for everyday Australians.
The RACGP is Australia’s peak body for general practice, representing over 28,500 GPs working in or towards a career in general practice.
Under the newly revised model, the Government has proposed a $5 cut in the GP patient rebate, a freeze to rebates until 2018 and an introduction of time-based changes to Level A consultations from 16 January 2015.
The RACGP labels these proposals as unacceptable.
Lots more is found here:
For more annoyance this has it all:
GP bodies defend co-pay policy response
16 December, 2014 Jo Hartley, Michael Woodhead and Kate Aubusson 103 comments
GP bodies have defended their muted reaction to the new co-payment plan that will strip $3.5 billion from general practice, as they prepare to meet with the Federal Health Minister.
Grass-roots GPs have blasted the AMA, RACGP and ACCRM for failing to hit out at the government for the savage cuts it plans to impose on general practice.
The overhaul, announced by Prime Minister Tony Abbott last Tuesday, saw the planned $7 co-payment for all patients axed.
But instead GPs will see $5 cut from rebates for non-concessional patients over 16, a freeze on all GP items until 2018 and an extension to the consult time for a level B item to a minimum of 10 minutes.
In their initial responses to the news, all three organisations welcomed the revised plan saying it was a win for vulnerable patients - with the AMA and the RACGP adding that they were "disappointed" by the cuts to general practice.
ACCRM President Dr Lucie Walters (pictured), however, went as far as to praise Mr Dutton for his "courage in taking a stand for quality and value for taxpayers’ money".
Later in the week the RACGP came out in support of the proposed changes to the level B rebate, saying in a statement it had "merit" because less than 10% of all consultations were six minutes long.
The college would "progress this initiative with government, which will come into force in a months time, it added.
Hundreds of doctors responded angrily on the Australian Doctor website, accusing the organisations of lacking bite and letting the profession down.
"This is purely an attack on GPs. The AMA are a non-representative GP mouth-piece, historically aligned with the Coalition. Where is the RACGP voice?" Dr David Moss wrote.
"The RACGP and its president has sold us out and the PM has insulted us by calling us 'sausage factory' medical practitioners after years of hard work and sacrifice," wrote a commentator known as Athanasius.
"I think enough is enough! The talk is over. Action is needed like never before. Proposal: Mass resignation from the college, and let them know why."
Lots more here:
Note the huge number if comments….
The lesson in all this is that medical politicians are like other politicians and can become rather disconnected with the interests of their members.
What offers hope is that the grassroots were listened to and appropriate responses emerged.
Make no mistake this is an ideological attack on the core concept and intent of Medicare as well as an outrageous attack on General Practice - and needs to be named as such and resisted.
I hear the AMA are preparing a campaign to run in all the practices around the country. If that is true and I was the Government I would be very, very worried.
If only it was as obvious just what a crock of an idea the PCEHR is!
Back to holidays!
David.
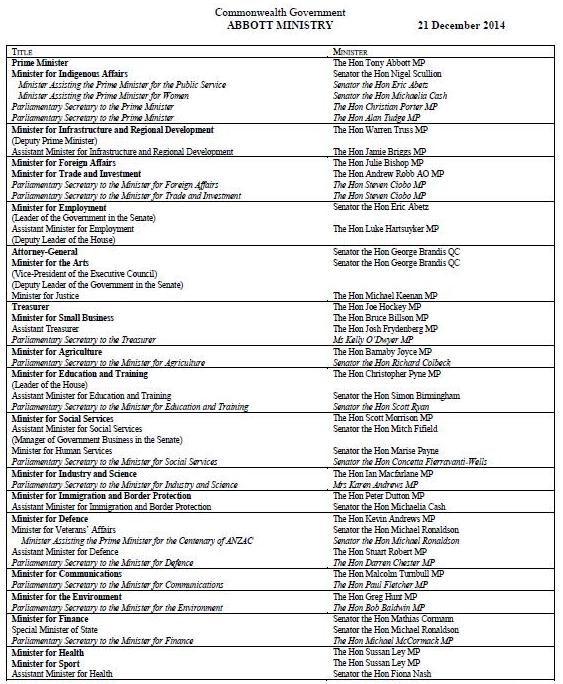
Big Changes In Federal Ministry! Peter Dutton Gets His Reward and Is Sent To Immigration!
Sussan Ley has been moved into Health.
Peter Dutton was clearly out of his depth in Health!
I wonder what will happen next?
She must be thrilled to have been given the unresolved PCEHR problem to fix!
David.
All the major details are here:
Tony Abbott has announced a cabinet reshuffle, promoting Scott
Morrison and dropping defence minister David Johnston in changes the
prime minister says will “refocus the government” on driving economic
reform next year.
Abbott described it as a “ministry for jobs and families” and said the government would be putting the economy at the centre of its agenda.
Morrison has been promoted to minister for social services. Abbott said Morrison was a “master of difficult policy” and that his ministry was “essentially a ministry for economic participation” that would encourage people “to give a fair go”.
Morrison will be responsible for crafting a “wholistic families package” that will be at the centre of the economic reform agenda next year. The move gives Morrison carriage of changes to Abbott’s controversial paid parental leave policy, which has been losing support among Coalition MPs.
Peter Dutton moves from health to immigration and border protection.
Sussan Ley takes Dutton’s previous role as health minister, becoming the second woman in Cabinet along with foreign minister Julie Bishop.
Full article here:
http://www.businessinsider.com.au/tony-abbott-cabinet-reshuffle-2014-12
D.
Full list:
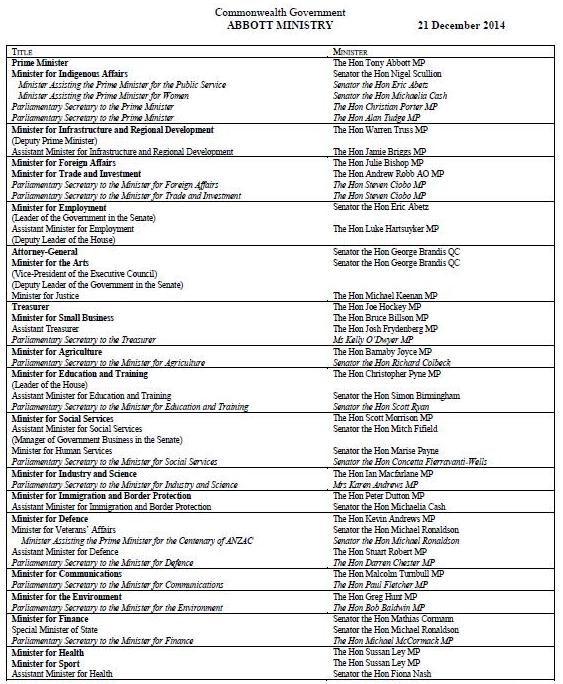
D.
Peter Dutton was clearly out of his depth in Health!
I wonder what will happen next?
She must be thrilled to have been given the unresolved PCEHR problem to fix!
David.
All the major details are here:
Australian Defence Minister Dumped From Office As Tony Abbott Reshuffles Cabinet
Abbott described it as a “ministry for jobs and families” and said the government would be putting the economy at the centre of its agenda.
Morrison has been promoted to minister for social services. Abbott said Morrison was a “master of difficult policy” and that his ministry was “essentially a ministry for economic participation” that would encourage people “to give a fair go”.
Morrison will be responsible for crafting a “wholistic families package” that will be at the centre of the economic reform agenda next year. The move gives Morrison carriage of changes to Abbott’s controversial paid parental leave policy, which has been losing support among Coalition MPs.
Peter Dutton moves from health to immigration and border protection.
Sussan Ley takes Dutton’s previous role as health minister, becoming the second woman in Cabinet along with foreign minister Julie Bishop.
Full article here:
http://www.businessinsider.com.au/tony-abbott-cabinet-reshuffle-2014-12
D.
Full list:
D.
AusHealthIT Poll Number 249 – Results – 21st December, 2014.
Here are the results of the poll.
Do You Think The Abbott Government is 'Strengthening Medicare' And Our Current Universal Healthcare System With The New Medicare Co-Payment Proposal?
For Sure 3% (2)Maybe 4% (3)
Neutral 13% (9)
Probably Not 13% (9)
No Way 65% (44)
I Have No Idea 1% (1)
Total votes: 68
A pretty clear response with large majority seeing through the suggestion that the Government is going to actually aid our Universal Healthcare System.
Good to see a clear outcome.
Again, many, many thanks to all those that voted!
David.
Friday, December 19, 2014
Happy Christmas And A Great 2015!
Well, that is your lot for the year unless we have some important news emerge of the 'silly season', that I feel an urgent need to post on.
I plan to re-start posting in mid to late Junuary 2015.
Till then stay safe and have a great break!
David.
I plan to re-start posting in mid to late Junuary 2015.
Till then stay safe and have a great break!
David.
Weekly Overseas Health IT Links - 20th December, 2014.
Note: Each link is
followed by a title and few paragraphs. For the full article click on the link
above title of the article. Note also that full access to some links may
require site registration or subscription payment.
-----
Argonaut Project is a Sprint Toward EHR Interoperability
Scott Mace, for HealthLeaders Media , December 9, 2014
The Argonaut Project that launched last week offers a real chance at much-needed workable EHR standards. But by itself, Argonaut won't lead to interoperability nirvana.
In Greek mythology,
the Argonauts, accompanied by heroic Jason, had to snatch a golden fleece from
a dragon who never slept. In 2015, the Argonaut Project aims to snatch a true interoperability
demonstration between EHR competitors and help healthcare providers who've
spent many a sleepless night trying to figure out how they can survive in this
new age of sharing EHR data.
Announced at last
week's HL7 Policy Conference in Washington, the Argonaut Project has the
backing of heavyweight EHR competitors Epic, Cerner, McKesson, Meditech, and
athenahealth, as well as heavy-hitting providers Partners HealthCare in Boston,
Intermountain Healthcare in Salt Lake City, Beth Israel Deaconess Medical
Center in Boston, and Mayo Clinic in Rochester, MN.
-----
Low Stage 2 Attestation Numbers Continue to Alarm
Greg Slabodkin
DEC 10, 2014 7:36am ET
Data from the
Centers for Medicare and Medicaid Services shows that as of Dec. 1, 2014, 1,681
hospitals and 16,455 eligible professionals have attested to Stage 2 meaningful
use.
That means less
than 35 percent of hospitals currently meet Stage 2 requirements and while
eligible professionals have until the end of February to report their progress,
only 4 percent of EPs have met Stage 2 requirements to date. The low
attestation numbers, presented during a Dec. 9 Health IT Policy Committee meeting, got the attention
of the College of Healthcare Information Management Executives which renewed
its call for CMS to immediately shorten the reporting period for 2015.
-----
FDA Presses Forward with Unique Device Identifier System
Greg Slabodkin and Greg Goth
DEC 11, 2014 7:52am ET
The U.S. Food and
Drug Administration is moving ahead with the Unique Device Identifier (UDI)
system to identify medical devices. Yet, the question remains: If FDA builds
the system, will the healthcare industry adopt it?
The agency is
working with manufacturers to launch the UDI system, which will be phased in
over several years. When fully implemented, the label of most medical devices
will include a unique device identifier in human- and machine-readable form. As
part of the implementation, device labelers will also submit certain
information about each device to FDA’s Global Unique Device Identification
Database, which the public will be able to search and download information.
Jeffrey Shuren,
M.D., director of the FDA’s Center for Devices and Radiological Health, says
that UDIs are “intended to streamline the monitoring of devices, improve safety
tracking and recall efficiency, and even make it easier to evaluate device
performance over time.” However, writing in a recent blog, Shuren acknowledges
that these benefits “will only become a reality when the UDI system is adopted
and integrated into the healthcare system—when
hospitals, doctors’ offices, patient registries, heathcare insurance companies,
and others incorporate UDI as part of their standard electronic health
information systems.”
-----
Healthcare Security In 2015: 9 Hotspots
12/10/2014 08:36 AM
With data breaches growing, 2015 promises to be
the healthcare industry's most challenging security year yet. These nine areas
demand attention in 2015.
Healthcare
organizations must tighten security or risk getting breached, penalized, and
potentially ostracized by a public fed up with seeming carelessness with their
personal information. Unfortunately, the task of securing protected health
information (PHI) is only becoming more challenging for even the best-prepared
organizations. Fitness bands, hospital portals, electronic health records,
health information exchanges, insurance networks -- the list of
Internet-connected devices, tools, and sites containing personal and medical
data keeps growing.
The healthcare
sector has been under attack for some time. In 2014, despite headlines
dominated by JPMorgan Chase, Home Depot, and other retail or financial
entities, the healthcare industry accounted for 43% of all major breaches,
according to the Ponemon Institute.
-----
Patients want more from their EHRs
Posted on Dec 11, 2014
By Mike Miliard, Editor
Having established
a level of trust and familiarity with electronic health records over the past
few years, increasing numbers of U.S. patients are looking for more advanced
features from their EHRs, according to a new survey from the National
Partnership for Women & Families.
The study, "Engaging
Patients and Families: How Consumers Value and Use Health IT," follows up
on a similar 2011 report that assessed consumer views toward EHRs. A lot has
changed since then, with more and more patients comfortable with the idea of
digitized records, and easier online access to health information spurring more
patient
engagement in their care.
In the past year,
more than four in five patients with online access to their health records (86
percent) used their online records at least once, according to NPWF; more than
half (55 percent) used them three or more times a year.
-----
Patients increasingly trust, value EHRs, survey finds
In the era of
patient engagement, patients are utilizing health IT tools to become more
active in their care.
Last year, 86
percent of patients used their EHR at least once, and 55 percent used them at
least three times a year, according to a study by National Partnership for
Women & Families.
The survey was a
follow-up to the organization's 2011 survey that aimed to assess consumer views
toward EHRs and health IT. The most recent survey repeated questions from the
2011 survey to identify and assess trends in consumer attitudes following
federal and state IT incentive programs, such as meaningful use.
-----
Health informatics job market in trouble
Posted on Dec 12, 2014
By Bernie Monegain, Editor-at-Large
"The demand
for health informatics workers is projected to grow at twice the rate of
employment overall, but there is strong evidence that the nation already faces
a shortage of qualified workers in this field," according to a new report
from research firm Burning Glass.
Moreover, the study
shows, job postings for health informatics personnel stay open long than others.
Employers are
struggling to fill many of these jobs, according to the Burning Glass. On
average, health informatics positions stay open for 35 days – two days longer
than the national average posting duration of 33 days.
-----
ONC Budget Remains Flat in FY15, $4B for VA
DEC 12, 2014 7:32am ET
The fiscal 2015
federal appropriations budget being finalized by Congress contains funds for
numerous health information technology initiatives under the Department
Veterans Affairs, Office of the National Coordinator for HIT and for rural
health, among other entities.
The Christmas time
bill is not particularly kind to ONC, granting a budget of $60, 367,000, the
same as in FY 2014. ONC had asked for $75 million in FY 2015, but the agency,
like others, generally requests more than it knows it will get.
In FY 2015, the
Small Rural Hospital Improvement Grant program is slated to get $14,942,000 for
quality improvement projects, adoption of telehealth services and coordinating
care between rural providers and VA’s VistA EHR, among other projects.
-----
True Interoperability: Public APIs provide the open platform health IT requires
Posted on Dec 09, 2014
By Edmund Billings, MD, Medsphere Systems Corporation
Do we finally have
the spark?
Interoperability is
the current health IT buzzword because it’s the essential ingredient in
creating a system that benefits patients, doctors and hospitals. Almost everyone
in healthcare is pressing for it and is frustrated, though probably not
surprised, that meaningful use did not get us
there.
The ONC says within
three years we’ll have a roadmap for providing interoperability “across vendor
platforms,” which should probably elicit a collective groan.
Look, a map is a
fine tool but of limited use if I don’t speak the language. Change in this
industry requires market drivers instituted now, if not sooner. We must move
from MU to a health care payment model driving True Interoperability, not the
garden-variety stuff.
-----
Interoperability Top Priority of Federal HIT Strategic Plan
Greg Slabodkin
DEC 10, 2014 7:45am ET
The 2015-2020
Federal Health IT Strategic Plan just
released by the Office of the National Coordinator
for HIT is about “collecting, sharing, and using electronic health
information,” according to Seth Pazinski, director of ONC’s Office of Planning,
Evaluation, and Analysis.
Pazinski told a
Dec. 9 meeting of the Health IT Policy Committee that the draft five-year plan
outlines the federal government’s many HIT priorities established by 35
participating agencies “but there was a coming together around interoperability
as a top focus and priority.”
Adopting the IEEE
definition of interoperability—the ability of two or more systems or components
to exchange information and to use the information that has been exchanged—the
plan argues that “interoperable health information and health IT solutions will
lead to more efficient and effective health systems, better clinical decision
support, scientific advancement, and a continuously learning health system.”
-----
ONC strategic plan raises questions about the future of Meaningful Use
December 10, 2014 | By Marla Durben Hirsch
The Office of the
National Coordinator for Health IT's updated
health IT strategic plan, released Dec. 8, is a high-level,
ambitious framework for the federal government. It addresses some of the
questions the industry has had about the direction of health IT and ONC. It's
also an interesting read.
The plans updated
goals include:
- Expand the adoption of health IT
- Advance secure and interoperable health
- Strengthen healthcare delivery
- Advance the health and wellbeing of individuals and communities
- Advance research, scientific knowledge and innovation
Clearly, the
strategic plan is a starting point, and the details still need to be hashed
out. But it raises a lot of questions in my mind.
-----
Phishing, ransomware attacks on health industry to rise
December 10, 2014 | By Susan D. Hall
While security
experts predict increased cyberattacks on healthcare organizations in 2015,
they foresee phishing and ransomware posing particular challenges.
Phishing emails try
to lure recipients into giving out information such as usernames, passwords or
credit card numbers. They also can give attackers ways to infiltrate the
enterprise network, according to an article in iHealthBeat by John
Moore of Chilmark.
"Phishing
emails often provide the entry point," Scott Koller, a lawyer at
BakerHostetler, says in the article.
-----
Medical Scribes May Ease EHR, ICD-10 Aches
Ryan Chiavetta, for HealthLeaders Media , December 10, 2014
Medical scribes offer hospitals and health systems a low-cost method to bolster productivity and boost physician efficiency and morale, particularly after an EHR implementation.
With the advent of
electronic health records in patient care, healthcare organizations have been
looking for a way to help physicians combat the deluge of mandates, while still
maintaining a high level of efficiency.
One fast-growing position designed to remedy this situation is the medical scribe. A medical scribe's primary duty is to document a physician's encounter with a patient in the electronic health record system. Scribes enter information about a patient's history, the physical exam, the physician's assessment, notes on decision making and discharge and after care instructions.
One fast-growing position designed to remedy this situation is the medical scribe. A medical scribe's primary duty is to document a physician's encounter with a patient in the electronic health record system. Scribes enter information about a patient's history, the physical exam, the physician's assessment, notes on decision making and discharge and after care instructions.
-----
Sutter Health Launches Online Tool for Teen Patients
Greg Goth
DEC 9, 2014 7:58am ET
Sacramento,
Calif.-based Sutter Health has launched My Health Online for Teens, an
electronic health service which provides teens secure, online access to their
health records and their doctors.
My Health Online
for Teens also provides a way for parents to stay connected with the doctor of
their teens, as their children learn how to manage their own healthcare. The
platform lets kids ages 12 to 17 email their doctors, review test results,
renew prescriptions, track immunizations, and schedule appointments from a
cellphone or laptop.
California law
requires that some aspects of a teen’s medical care, particularly reproductive
and substance abuse services, be kept confidential once the child turns 12.
Rather than block parental access to the record entirely, in the Sutter
platform teens get full access to their personal health records. They can send
confidential questions or concerns directly to their doctors and view their
health data online.
------
For healthcare, Google Glass still has it
Posted on Dec 09, 2014
By Frank Irving, Editor, Medical Practice Insider
There's plenty of potential for Google Glass in healthcare, despite
reports that have called into question the technology's value.
"Glass in the enterprise is certainly stronger than it's ever
been. Google is investing very heavily," said Kyle Samani, CEO of
Pristine, a company that develops software for the device, during a Monday
afternoon session at the mHealth
Summit outside Washington, D.C.
Samani was part of
a panel that included Paul Porter, MD, director of special projects and
telemedicine for Brown University Emergency Medicine, and Sean Lunde, mHealth
lead for Wipro's healthcare and life sciences consulting group. They noted
several use cases where Google Glass is being tested
-----
EHI Awards 2014: Rising star
Claire Read speaks to Dave Newton, the winner of the first ‘rising
star’ category of the EHI Awards, about his work on the myhealthlocker project
for South London and Maudsley NHS Foundation Trust.
8 December 2014
“I didn’t
originally start out with a big plan of going into healthcare informatics,”
admits Dave Newton, the winner of the ‘rising star’ category of the EHI Awards
2014.
In fact, his
initial career plan was to become a clinical psychologist. When health IT came
calling, he was working as a researcher at South London and Maudsley NHS
Foundation Trust, exploring the concept of recovery in older adults suffering
from mental ill health.
“I was speaking at
a conference about recovery,” he remembers. “And one of the professors from the
Institute of Psychiatry was talking around something called avatar therapy, which
they were just starting to pilot.
-----
ICD-10 Delay Could Be Data Disaster
by The
Coalition for ICD-10 Tuesday, December 9, 2014
Earlier this year,
Congress enacted a one-year delay of the implementation of ICD-10-CM/PCS code
sets, extending the date from October 2014 to October 2015. This delay was
characterized by some as a bump in the road on the way to better health care
data.
Now, with some
physician groups advocating for an additional delay of up to two more years,
it's time for the industry to recognize that such obstruction is more than a
bump in the road. If the health care industry continues to delay ICD-10
implementation, we are careening toward a health care data disaster. Given that
the current system in use, ICD-9-CM/PCS, is inadequate for present-day uses and
that past delays have incurred significant costs, further delays will have
catastrophic consequences for the industry, with no measurable benefit. The
health care industry simply cannot afford any more delays in ICD-10
implementation.
-----
Data Breaches to Continue to Plague Healthcare in 2015
Greg Slabodkin
DEC 8, 2014 7:23am ET
The healthcare
industry will continue to be a vulnerable and attractive target for
cybercriminals in 2015, thanks to the expanding number of access points to
protected health information and other sensitive data via electronic health
records and the growing popularity of wearable technology.
That’s the
conclusion of Experian’s second annual Data Breach Industry Forecast, which
predicts that healthcare will continue to be plagued with data breaches in
2015. Healthcare organizations accounted for about 42 percent of all major data
breaches reported in 2014. “We expect this number will continue to grow until
the industry comes up with a stronger solution to improve its cybersecurity
strategies,” said Michael Bruemmer, vice president at Experian Data Breach Resolution,
in a written statement.
“Healthcare
organizations face the challenge of securing a significant amount of sensitive
information stored on their network, which combined with the value of a medical
identity string makes them an attractive target for cybercriminals,” states the
report. “The problem is
further exasperated by the fact that many doctors’ offices, clinics and
hospitals may not have enough resources to safeguard their patients’ PHI.”
-----
ONC's Five-Fold Federal Health IT Plan Looks Beyond EHRs
December 8, 2014 by Gabriel Perna
Karen DeSalvo, M.D.
The Office of the National Coordinator for Health IT (ONC) released
a five-fold federal health IT strategic plan, which focuses on widespread
health data sharing and looks beyond adoption of electronic health record (EHR)
systems.
The ONC's five-fold plan does include the expansion of health IT
adoption, particularly in the long-term care sector, but it also features the
advancement of an interoperable infrastructure, the strengthening of the
healthcare delivery system, the advancement of well-being of individuals and
communities, and the advancement of scientific research. The first two,
expansion of health IT adoption and advancement of interoperable
infrastructure, are the top priorities, says ONC. All of them require some kind
of interoperability push.
On a call announcing the plan, Karen DeSalvo, M.D., the National
Coordinator for Health IT, confirmed that there was a "big push for
interoperability" with this latest plan.
-----
ONC updates Health IT Strategic Plan
Posted on Dec 08, 2014
By Mike Miliard, Editor
The Office of the
National Coordinator for Health IT on Monday announced the release of its Federal Health IT
Strategic Plan, 2015-2020, updating the goals of an initiative most
recently released in 2011.
As it maps out ways
to better gather, share and put to use interoperable health data, the plan will
serve as a broad federal strategy, say ONC officials, helping
set the context for the Nationwide Interoperability Roadmap, which is
scheduled to be released January 2015.
That roadmap will
help to define the implementation of how the federal government can work with
the private sector to spur more widespread sharing of health data to improve
individual healthcare, drive better community and public health and advance
research.
-----
New goals in national HIT roadmap
By Mike Miliard, Contributing Editor
The Office of the
National Coordinator for Health IT has outlined its Federal Health IT
Strategic Plan, 2015-2020, updating the
goals of an initiative most recently released in 2011.
As it maps out ways
to better gather, share and put to use interoperable health data, the plan will
serve as a broad federal strategy, say ONC officials, helping set the
context for the Nationwide Interoperability Roadmap, which is
scheduled to be released January 2015.
That roadmap will
help to define the implementation of how the federal government can work with
the private sector to spur more widespread sharing of health data to improve
individual healthcare, drive better community and public health and advance
research.
-----
ONC updated HIT plan focuses on interoperability
December 8, 2014 | By Katie Dvorak
The Office of the
National Coordinator for Health IT's updated Federal Health IT Strategic
Plan, released today and spanning from 2015 to
2020, will focus on the collection, use and sharing of interoperable health
information.
The plan
"serves as the broad federal strategy setting the context and framing the
Nationwide Interoperability Roadmap that will be released in early 2015,"
according to an announcement from ONC.
In addition to
interoperability, the plan focuses on patient-generated data.
-----
At the mHealth Summit: Sensors, watches and glasses, oh my!
December 8, 2014 | By Susan D. Hall
The mHealth Summit
kicked off Sunday at Maryland's National Harbor with provider engagement and
integration of mobile health technologies into healthcare among the major
themes.
"I believe we
will see mHealth devices become even more ubiquitous, driven by non-health-related
consumer companies--whom we can learn a great deal from in terms of making
health and wellness a part of our day-to-day lives," Rich Scarfo, director
of the event and vice president of its backer, the Personal Connected Health
Alliance, says at mHealth News.
A range of
stakeholders will chime in, including consumer electronics giants, pharmacy
chains and life sciences companies.
-----
California hospital’s patient safety protocols now require a wearable
A California hospital has begun requiring certain patients use a
wearable remote patient monitoring device in order to comply with internal
patient safety protocols. Chino Valley Medical Center is employing the Leaf Patient Monitoring System from
Pleasanton-based Leaf Healthcare.
The sensor monitors
patient movement in bed, then uses that data to calculate when the patient
needs to be turned to prevent the formation of pressure ulcers. That data
is uploaded wirelessly to central monitoring stations or mobile devices so
clinicians can monitor the readings. The system also alerts nurses or staff when
a patient needs to be turned.
A recent clinical
trial showed that use of the sensor increased compliance with hospital turn
procedures from a baseline 64 percent to 98 percent. Ulcers are a dangerous and
painful condition which cost the US healthcare system $11 billion a year according to AHRQ, and because
they’re hospital-acquired, treatment is often not reimbursable by
insurers.
-----
Alberta moves on integrated health records system
Published on: December 5, 2014Last Updated: December 5, 2014 9:52 PM
MST
Alberta’s Health
Minister has struck a task force to investigate the creation of an integrated
provincial health information system after the College of Physicians and
Surgeons told a legislature committee this week the current system is “woefully
inadequate.”
Stephen Mandel has
chosen Alberta Health Services administrator Carl Amrhein to lead the task
force to look into the business case for a provincial clinical information
system and report back early in the new year, Mandel’s spokesman Steve Buick
said Friday.
“This is a group to
take a first look at it for the minister and get back to him quickly,” he said.
“The thinking is we need a single provincial system.”
-----
http://www.modernhealthcare.com/article/20141208/NEWS/312089928
New federal health IT plan emphasizes adoption, interoperability
The Office of the
National Coordinator for Health Information Technology has adopted a new
strategic plan that seeks to keep up the momentum of health IT adoption while
taking steps to improve the penetration of information technology beyond
hospitals and physician practices.
Under the American
Recovery and Reinvestment Act's electronic health-record incentive payment
program, which has paid out nearly $25.8 billion since 2011, 94% of eligible
hospitals and 79% of eligible physicians have received payment for either
purchasing or meaningfully using a tested and certified EHR.
But the program
left gaps by not extending payments to behavioral health, long-term care and
other providers, said Dr. Karen DeSalvo, head of the ONC.
The ONC and other federal agencies are looking at ways to help these excluded
providers cover the cost of buying EHRs.
-----
Enjoy!
David.