The following is a letter I e-mailed to Minister Tony Abbott a little over a week ago. In the covering note I pointed out I would like a response and that I planned to publish the letter on this site after a week or two.
-----------
An Open Letter to Minister Tony Abbott.
11th March 2007
The Hon Tony Abbott MP
Leader of the House; Minister for Health and Ageing.
PO Box 6022
House of Representatives
Parliament House
Canberra ACT 2600
Dear Mr Abbott,
The Australian health system is not as safe, as efficient or as cost effective as it could and should be.
A major, but not the only reason for this is that the health sector is not using proven Information and Communication Technology effectively in order to get the benefits which have been received by virtually all other sectors of the Australian economy.
I believe this is a major policy failure of the present Government and will have electoral consequences unless addressed promptly with a coherent, inclusive and properly funded National Health IT Strategy in conjunction with an appropriate Business Plan and Implementation Strategy. Neither NEHTA nor the newly re-formed Australian Health Information Council appear to be cognisant of and focussed upon the excess costs and suffering inaction is causing. Action is required promptly.
There will be electoral consequences due to the public perceptions of wastage of many dollars on the current strategy, the lack of transparency in the evaluation and reporting of what has been achieved to date, the recognition we are slipping well behind other countries (e.g. the UK, Canada and the Netherlands) and the unacceptable number of otherwise avoidable deaths and injuries due to unsafe and inadequate systems.
The net benefits of successful implementation of such a plan would conservatively be at least five percent of national health expenditure ($4 Billion per annum), if overseas research from the US, the UK and Canada are any guide.
I have developed an internet web-log containing over 140 articles on this topic over the last 12 months and I have exposed my thinking to public criticism and review. I have found that the 200 plus expert readers are typically very supportive of my suggestions in the Health IT domain.
I would be pleased to have your officials browse my web-log for a well considered and developed set of ideas and approaches on what is needed to recruit the benefits and to move Australia forward in this very important area.
The web-log can be viewed at http://www.aushealthit.blogspot.com/ .
Yours truly,
- Signed -
(Dr) David More MB, PhD, FACHI.
----------
As of the time of posting no response has been received from the minister
David.
This blog is totally independent, unpaid and has only three major objectives.
The first is to inform readers of news and happenings in the e-Health domain, both here in Australia and world-wide.
The second is to provide commentary on e-Health in Australia and to foster improvement where I can.
The third is to encourage discussion of the matters raised in the blog so hopefully readers can get a balanced view of what is really happening and what successes are being achieved.
Quote Of The Year
Timeless Quotes - Sadly The Late Paul Shetler - "Its not Your Health Record it's a Government Record Of Your Health Information"
or
H. L. Mencken - "For every complex problem there is an answer that is clear, simple, and wrong."
Sunday, March 18, 2007
An Open Letter to Minister Tony Abbott.
Thursday, March 15, 2007
The Shared EHR – Can it Be Done Simply and Make a Difference?
In this short article I want to raise, and attempt to solve at a high level, some of the problems associated with the currently proposed Shared Electronic Health Record (SEHR).
The reason to document this is that in its latest presentations NEHTA is still saying it wants to put a business case for implementation of a National SEHR to the Council of Australian Government by the end of 2008.
What I mean by a SEHR is an arrangement (in its most simple form) where by a variety of feeder systems found in general practice, specialist offices, hospitals and services such as labs, pharmacies and radiology create summary records as they process patients which are then uploaded to a central repository. These summaries are envisaged to accumulate over the life of the patient to form a valuable longitudinal electronic patient record.
The central repository is then accessible to authorised users to assist with the care of the individual patient at some time later.
With minor tweaking around the edges the NEHTA proposal seems to be a re-run of the late 2004 HealthConnect project which was a month or two after that date placed into development limbo. The most evolved public version of the HealthConnect proposal was the Version 1.9 of its proposed Business Architecture (BA).
There do exist some slightly later NEHTA documents providing a “Concept of Operations” for a NEHTA SEHR but these are not publicly available.
It must be reasonably obvious to all that creation of a nation SEHR is not a uncomplicated exercise – indeed, since proposed in late 2001 – very considerable work has been done, pilots of components have been undertaken but any really extensible or expandable success simply has not been demonstrated. Those with a historical bent can follow all this is excruciating detail at the following URL:
http://www.health.gov.au/internet/hconnect/publishing.nsf/Content/home
This site was last updated 17 Feb, 2006.
I will state a prejudice here and state I think the SEHR of the BA Version 1.9 and NEHTA’s present plans are probably too complex, when fully analysed, to be made reality. That said I believe there is the possibility of doing something very clinically useful if those responsible stand back and work out clearly where information should be stored and processed within the health system.
What I suggest is that a practical approach to the SEHR should be a very simple base record – held voluntarily in a central repository - that contains the information that may change the way an individual is treated in the first day or so of an encounter with an emergency facility, hospital or new doctor. If that can be made to work, then, and only then, should consideration be given to doing more in a shared EHR sense.
There are a number of templates available for what to me should be a single form which is stored centrally and updated by the patient and their attending doctor at each appropriate encounter. All that would be stored would be essentially patient demographics, major current illnesses and problems, allergies and current medications, with maybe some free text for special items of warning or alert.
The standard of information I would suggest is appropriate is the amount of information a thorough GP would provide about a patient who as going for an overseas trip where they may need care from a doctor who had never seen them before.
If more detail is required, it is at that point reference is made to the owners of the patient’s detailed information – e.g. laboratory providers, specialists, local GP etc.
Any design that attempts more than this simple approach (of voluntary sharing of a basic information set agreed between the patient and their usual clinical adviser) will get tangled up with a range of issues.
These include:
• Concerns for privacy and lack of control of their personal information on the part of the consumer / patient
• Difficulties and delays in delivery of a workable system due to complexity if a more adventurous approach is attempted.
• Excessive cost in infrastructure requirements.
It seems to me such a basic standardised record would typically be able to be relatively easily read and created by quality GP and other relevant systems – and a secure messaging solution to and from a central repository would not be too difficult to devise within current standards.
Either the Access Card Identifier or the NEHTA Health IHI could be used to safely identify patients if either is available, or an alternative devised if required. Only one would be needed.
Under my approach all the heavy computational lifting – that promotes quality and safety in clinical care – would be done within client systems in the General Practice, Specialist’s Office or Hospital where clinicians engage with the details of care and where decision support is most valuable.
Such a model of a simple shared record and quality computing for the clinical workface (i.e. Local EHR) I find intrinsically appealing and doable today. I hope something practical, quickly implementable and workable emerges from NEHTA’s deliberations in this area.
I am firmly of the ‘walk before you run’ school in Health IT. Round the world we see simplification working and complexity confounding the most energetic. Let’s grasp that lesson and move forward.
David.
The reason to document this is that in its latest presentations NEHTA is still saying it wants to put a business case for implementation of a National SEHR to the Council of Australian Government by the end of 2008.
What I mean by a SEHR is an arrangement (in its most simple form) where by a variety of feeder systems found in general practice, specialist offices, hospitals and services such as labs, pharmacies and radiology create summary records as they process patients which are then uploaded to a central repository. These summaries are envisaged to accumulate over the life of the patient to form a valuable longitudinal electronic patient record.
The central repository is then accessible to authorised users to assist with the care of the individual patient at some time later.
With minor tweaking around the edges the NEHTA proposal seems to be a re-run of the late 2004 HealthConnect project which was a month or two after that date placed into development limbo. The most evolved public version of the HealthConnect proposal was the Version 1.9 of its proposed Business Architecture (BA).
There do exist some slightly later NEHTA documents providing a “Concept of Operations” for a NEHTA SEHR but these are not publicly available.
It must be reasonably obvious to all that creation of a nation SEHR is not a uncomplicated exercise – indeed, since proposed in late 2001 – very considerable work has been done, pilots of components have been undertaken but any really extensible or expandable success simply has not been demonstrated. Those with a historical bent can follow all this is excruciating detail at the following URL:
http://www.health.gov.au/internet/hconnect/publishing.nsf/Content/home
This site was last updated 17 Feb, 2006.
I will state a prejudice here and state I think the SEHR of the BA Version 1.9 and NEHTA’s present plans are probably too complex, when fully analysed, to be made reality. That said I believe there is the possibility of doing something very clinically useful if those responsible stand back and work out clearly where information should be stored and processed within the health system.
What I suggest is that a practical approach to the SEHR should be a very simple base record – held voluntarily in a central repository - that contains the information that may change the way an individual is treated in the first day or so of an encounter with an emergency facility, hospital or new doctor. If that can be made to work, then, and only then, should consideration be given to doing more in a shared EHR sense.
There are a number of templates available for what to me should be a single form which is stored centrally and updated by the patient and their attending doctor at each appropriate encounter. All that would be stored would be essentially patient demographics, major current illnesses and problems, allergies and current medications, with maybe some free text for special items of warning or alert.
The standard of information I would suggest is appropriate is the amount of information a thorough GP would provide about a patient who as going for an overseas trip where they may need care from a doctor who had never seen them before.
If more detail is required, it is at that point reference is made to the owners of the patient’s detailed information – e.g. laboratory providers, specialists, local GP etc.
Any design that attempts more than this simple approach (of voluntary sharing of a basic information set agreed between the patient and their usual clinical adviser) will get tangled up with a range of issues.
These include:
• Concerns for privacy and lack of control of their personal information on the part of the consumer / patient
• Difficulties and delays in delivery of a workable system due to complexity if a more adventurous approach is attempted.
• Excessive cost in infrastructure requirements.
It seems to me such a basic standardised record would typically be able to be relatively easily read and created by quality GP and other relevant systems – and a secure messaging solution to and from a central repository would not be too difficult to devise within current standards.
Either the Access Card Identifier or the NEHTA Health IHI could be used to safely identify patients if either is available, or an alternative devised if required. Only one would be needed.
Under my approach all the heavy computational lifting – that promotes quality and safety in clinical care – would be done within client systems in the General Practice, Specialist’s Office or Hospital where clinicians engage with the details of care and where decision support is most valuable.
Such a model of a simple shared record and quality computing for the clinical workface (i.e. Local EHR) I find intrinsically appealing and doable today. I hope something practical, quickly implementable and workable emerges from NEHTA’s deliberations in this area.
I am firmly of the ‘walk before you run’ school in Health IT. Round the world we see simplification working and complexity confounding the most energetic. Let’s grasp that lesson and move forward.
David.
Sunday, March 11, 2007
Three Years Too Late – NEHTA Asks What’s Next?
A few days ago I heard about an 80 minute Panel Session that NEHTA is planning to conduct on 20 March 2007. (The date is one day before the Health E-Nation Conference being organised by CHIK Services on 21 March)
The information I received is as follows:
_________________________________
“Planned Panel Session
Title
Joining the Dots… What’s Next
Aims
To identify the priority areas for action to enable e-reforms to progress to national implementation.
To identify the most significant outstanding obstacles to progress and what must be done in the next 12 months to address these priority issues.
To enjoy a lively discussion with questions and comments from the audience.
Interview questions
What do you believe are the 1 or 2 key areas for action over the next 2 to 3 years? Please give brief, specific examples to illustrate your points.
What do you believe is the single most important thing we need to do to accelerate e-health in the next 12 months from the point of view of health consumers or patients? And also from the point of view of health professionals?
What is your organisation currently doing to accelerate e-health reforms? Example?
Is there any other significant issue you would like to raise?”
_______________________
I was also told it is planned there will be panellists from six to eight different relevant organisations.
What is to be made of this?
My first reaction was to ask – Why was this work, which is essentially aimed at setting strategic and short term directions, not undertaken three years ago?
Then it occurred to me ponder – hang on – isn’t NEHTA meant to be managing the delivery and implementation of e-Health in Australia? How is it they don’t know the answers to all these questions as part of their strategic plan? If the aim of this Planned Panel Session is to confirm current directions I would be re-assured – but for NEHTA to now be asking what the priorities and barriers are at this point – three years into the mission – seems just quite absurd.
As readers of this blog will know I have been banging on about the need for an action orientated National E-Health Strategy, Business Case and Implementation Plan for a good while now! My answer to NEHTA’s request therefore is quite straightforward. Put simply what NEHTA has to do is as follows:
1. Recognise that their customer is not the NEHTA Board but the Australian Health Sector, and the 20 million people who use the services provided by it.
2. Swiftly enrol competent expertise and find the resources and funds to develop a consultative, inclusive, National E-Health Strategy, Business Case and Implementation Plan.
3. Use the Business Case to secure the appropriate level of funding required to move forward
4. Implement the agreed and recommended plan nationally.
I have had a feeling in the last few months that I have been missing something, else we would be seeing more constructive activity than seems to be the case. I have formed the view that the lack of an agreed national strategy is fundamentally a major obstacle to progress. Broadly speaking what I think we are now seeing is the following:-
1. State Governments working to use Health IT to try to get their hospitals working better (albeit with different levels of success and urgency) and starting to try and communicate with the relevant GPs and Specialists.
2. Most GPs and Specialists lacking the motivation (or the right incentives and support) to move beyond basic practice computing and prescription printing until future directions become clearer. (Note: there are all sorts of good things happening at many Divisions but somehow the task of co-ordinating information and skill sharing seems less than ideal).
3. The medical software industry is responding where it can but it lacks confidence in the stability of the direction being taken and the preparedness by Government(s) and practitioners to invest.
4. Service providers (labs, radiology etc) are optimising internal operations and providing external messaging of results etc largely only when asked. Electronic ordering is still at a low level.
5. A significant and consistent lack of support for implementation of already developed standards as well as some caution around standards which exist on paper but are not yet demonstrably implemented.
6. An evolving but still non-interoperable secure electronic messaging environment which lacks certainty in the forward directions that will be successful resulting in slow investment and complexity of use for end users.
7. A clear sense that the HealthConnect proposal(s) is/are going no-where in the next 3-4 years at best and that in reality HealthConnect has been canned.
8. Scepticism regarding announcements in areas such as e-prescribing, supply chain and medicine terminology among others.
Development of a comprehensive National E-Health Plan can, if funded and sponsored at the right level, provide the confidence, financial security and direction to get over the log-jam.
There are a few critical requirements for national E-Health Plans to be successful. These include at least the following:
1. That the plan be designed for the way the Health Sector in a country works in terms of funding, service delivery and so on. The implication is that what is done in the US, UK, Canada or Europe will only offer ideas – not a comprehensive solution.
2. That the plan, once developed, be sponsored, funded and committed to on a bi-partisan national interest motivated mode. Implementation of a plan of the type required is a major long term project and as far as possible politicisation needs to be avoided.
3. The plan be conceived to address the health system as a whole – and not fall into all the traps of Commonwealth / State rivalry, friction etc.
4. Inclusiveness of all the relevant stakeholders (Consumers, Providers, Government, Health Funds etc)
5. Focussed on delivery of clinical benefits for patients along with facilitation of health sector safety, efficiency and effectiveness.
6. Recognition that the benefits from the use of Health IT are often not captured by those whose work practices are changed and who may also bear additional costs.
7. Recognition that significant incentives for change will be required.
8. Recognition that Health IT is an enabler of Health Sector Reform and Improvement and that leadership of and commitment to Health System redesign is also needed.
There are a number of major strategic choices that also need to be made. Among these are (in no particular order – they are all crucial):
1. The level of standardisation that is to be imposed and at what level(s) this is to happen – as there is a trade off between user choice and the degree of inter-operation and information sharing that can be achieved without undue complexity.
2. Whether the approach to development and implementation will be ‘top down’ (as broadly it is in the UK) or ‘bottom up’ (as broadly it is in the US). This will ultimately drive a strategic E-Health Architecture for the county and the route by which that architecture will be evolved in practice.
3. The respective place and role(s) of the Government(s), the health service providers, the private sector software industry and so on the overall mix of how things are achieved.
4. Whether a Shared EHR or a messaging paradigm will be adopted and whether a distributed or centralised model will be adopted. There are a huge range of shades of choice that may be made in this area.
5. The suite of standards that will be utilised and how compliance with those standards will be obtained, certified and maintained.
6. The level of local and regional autonomy that will be available and the areas of the strategy where this will operate.
7. The amount of system development, service provision etc that will be undertaken centrally by Government(s) versus the use of commercially provided software and services.
8. The approach to risk management and to issues such as the verification of solution suitability and piloting of proposed solutions.
9. The funding model to be adopted and the approach to be adopted to benefits identification, management, realisation and distribution.
10. What is preferred and the optimal method of software provider and user / public / consumer involvement in the selection, deployment and use of Health IT and what consultative approach should be used in development of the strategy.
11. The strategies to be used in gaining public confidence regarding the privacy and security of their personal health information.
12. How best to take most advantage of the useful work undertaken to date in the field, while not constraining an optimal long term outcome for Australia.
13. The optimal governance framework and management structure for delivery of such a large and complex national initiative.
The benefits of providing clarity to all stakeholders on the shape of the future and the part they can play in advancing towards that future are obvious in terms of the levels of investment and benefits that will flow.
The best thing that could happen would be that the new AHIC and NEHTA jointly approach COAG / AHMAC to get such a planning process initiated as soon as possible.
I wonder whether those bodies have the ‘intestinal fortitude’ needed to step back, accept we are not getting anywhere fast, and initiate a new planning process.
I am reminded of the following quote:
There is a tide in the affairs of men,
Which, taken at the flood, leads on to fortune;
Omitted, all the voyage of their life
Is bound in shallows and in miseries.
William Shakespeare, Julius Caesar
Greatest English dramatist & poet (1564 - 1616)
The tide is rising right now!
David.
The information I received is as follows:
_________________________________
“Planned Panel Session
Title
Joining the Dots… What’s Next
Aims
To identify the priority areas for action to enable e-reforms to progress to national implementation.
To identify the most significant outstanding obstacles to progress and what must be done in the next 12 months to address these priority issues.
To enjoy a lively discussion with questions and comments from the audience.
Interview questions
What do you believe are the 1 or 2 key areas for action over the next 2 to 3 years? Please give brief, specific examples to illustrate your points.
What do you believe is the single most important thing we need to do to accelerate e-health in the next 12 months from the point of view of health consumers or patients? And also from the point of view of health professionals?
What is your organisation currently doing to accelerate e-health reforms? Example?
Is there any other significant issue you would like to raise?”
_______________________
I was also told it is planned there will be panellists from six to eight different relevant organisations.
What is to be made of this?
My first reaction was to ask – Why was this work, which is essentially aimed at setting strategic and short term directions, not undertaken three years ago?
Then it occurred to me ponder – hang on – isn’t NEHTA meant to be managing the delivery and implementation of e-Health in Australia? How is it they don’t know the answers to all these questions as part of their strategic plan? If the aim of this Planned Panel Session is to confirm current directions I would be re-assured – but for NEHTA to now be asking what the priorities and barriers are at this point – three years into the mission – seems just quite absurd.
As readers of this blog will know I have been banging on about the need for an action orientated National E-Health Strategy, Business Case and Implementation Plan for a good while now! My answer to NEHTA’s request therefore is quite straightforward. Put simply what NEHTA has to do is as follows:
1. Recognise that their customer is not the NEHTA Board but the Australian Health Sector, and the 20 million people who use the services provided by it.
2. Swiftly enrol competent expertise and find the resources and funds to develop a consultative, inclusive, National E-Health Strategy, Business Case and Implementation Plan.
3. Use the Business Case to secure the appropriate level of funding required to move forward
4. Implement the agreed and recommended plan nationally.
I have had a feeling in the last few months that I have been missing something, else we would be seeing more constructive activity than seems to be the case. I have formed the view that the lack of an agreed national strategy is fundamentally a major obstacle to progress. Broadly speaking what I think we are now seeing is the following:-
1. State Governments working to use Health IT to try to get their hospitals working better (albeit with different levels of success and urgency) and starting to try and communicate with the relevant GPs and Specialists.
2. Most GPs and Specialists lacking the motivation (or the right incentives and support) to move beyond basic practice computing and prescription printing until future directions become clearer. (Note: there are all sorts of good things happening at many Divisions but somehow the task of co-ordinating information and skill sharing seems less than ideal).
3. The medical software industry is responding where it can but it lacks confidence in the stability of the direction being taken and the preparedness by Government(s) and practitioners to invest.
4. Service providers (labs, radiology etc) are optimising internal operations and providing external messaging of results etc largely only when asked. Electronic ordering is still at a low level.
5. A significant and consistent lack of support for implementation of already developed standards as well as some caution around standards which exist on paper but are not yet demonstrably implemented.
6. An evolving but still non-interoperable secure electronic messaging environment which lacks certainty in the forward directions that will be successful resulting in slow investment and complexity of use for end users.
7. A clear sense that the HealthConnect proposal(s) is/are going no-where in the next 3-4 years at best and that in reality HealthConnect has been canned.
8. Scepticism regarding announcements in areas such as e-prescribing, supply chain and medicine terminology among others.
Development of a comprehensive National E-Health Plan can, if funded and sponsored at the right level, provide the confidence, financial security and direction to get over the log-jam.
There are a few critical requirements for national E-Health Plans to be successful. These include at least the following:
1. That the plan be designed for the way the Health Sector in a country works in terms of funding, service delivery and so on. The implication is that what is done in the US, UK, Canada or Europe will only offer ideas – not a comprehensive solution.
2. That the plan, once developed, be sponsored, funded and committed to on a bi-partisan national interest motivated mode. Implementation of a plan of the type required is a major long term project and as far as possible politicisation needs to be avoided.
3. The plan be conceived to address the health system as a whole – and not fall into all the traps of Commonwealth / State rivalry, friction etc.
4. Inclusiveness of all the relevant stakeholders (Consumers, Providers, Government, Health Funds etc)
5. Focussed on delivery of clinical benefits for patients along with facilitation of health sector safety, efficiency and effectiveness.
6. Recognition that the benefits from the use of Health IT are often not captured by those whose work practices are changed and who may also bear additional costs.
7. Recognition that significant incentives for change will be required.
8. Recognition that Health IT is an enabler of Health Sector Reform and Improvement and that leadership of and commitment to Health System redesign is also needed.
There are a number of major strategic choices that also need to be made. Among these are (in no particular order – they are all crucial):
1. The level of standardisation that is to be imposed and at what level(s) this is to happen – as there is a trade off between user choice and the degree of inter-operation and information sharing that can be achieved without undue complexity.
2. Whether the approach to development and implementation will be ‘top down’ (as broadly it is in the UK) or ‘bottom up’ (as broadly it is in the US). This will ultimately drive a strategic E-Health Architecture for the county and the route by which that architecture will be evolved in practice.
3. The respective place and role(s) of the Government(s), the health service providers, the private sector software industry and so on the overall mix of how things are achieved.
4. Whether a Shared EHR or a messaging paradigm will be adopted and whether a distributed or centralised model will be adopted. There are a huge range of shades of choice that may be made in this area.
5. The suite of standards that will be utilised and how compliance with those standards will be obtained, certified and maintained.
6. The level of local and regional autonomy that will be available and the areas of the strategy where this will operate.
7. The amount of system development, service provision etc that will be undertaken centrally by Government(s) versus the use of commercially provided software and services.
8. The approach to risk management and to issues such as the verification of solution suitability and piloting of proposed solutions.
9. The funding model to be adopted and the approach to be adopted to benefits identification, management, realisation and distribution.
10. What is preferred and the optimal method of software provider and user / public / consumer involvement in the selection, deployment and use of Health IT and what consultative approach should be used in development of the strategy.
11. The strategies to be used in gaining public confidence regarding the privacy and security of their personal health information.
12. How best to take most advantage of the useful work undertaken to date in the field, while not constraining an optimal long term outcome for Australia.
13. The optimal governance framework and management structure for delivery of such a large and complex national initiative.
The benefits of providing clarity to all stakeholders on the shape of the future and the part they can play in advancing towards that future are obvious in terms of the levels of investment and benefits that will flow.
The best thing that could happen would be that the new AHIC and NEHTA jointly approach COAG / AHMAC to get such a planning process initiated as soon as possible.
I wonder whether those bodies have the ‘intestinal fortitude’ needed to step back, accept we are not getting anywhere fast, and initiate a new planning process.
I am reminded of the following quote:
There is a tide in the affairs of men,
Which, taken at the flood, leads on to fortune;
Omitted, all the voyage of their life
Is bound in shallows and in miseries.
William Shakespeare, Julius Caesar
Greatest English dramatist & poet (1564 - 1616)
The tide is rising right now!
David.
Yes, It Really Can be Done!
Just a short posting to provide a URL for a fascinating ten minute downloadable video that explains what the Dutch have been up to in e-Health over the last few years!
The video describes AORTA which is the Dutch national infrastructure for the exchange of data between healthcare providers. The infrastructure specifications include a description of technical, organizational as well as implementation aspects. The focus of this program is to facilitate the realization of a national "continuity of care" oriented EHR. AORTA uses HL7 version 3 messages and documents as its core mechanism for information exchange.
Depending on your media preference you have a choice of formats.
AORTA introductory video (in English, 10 minutes),
http://www.uzi-register.nl/media/EMD_WDH_EN_256K.wmv (Windows Media file)
or
http://www.uzi-register.nl/media/EMD_WDH_EN_H264%20.mov (Apple Quicktime).
Vastly more information and detail on the project can be found at:
http://www.ringholm.de/docs/00980_en.htm
The author is René Spronk - Sr.Consultant, Ringholm GmbH
The current document status: Draft, version 0.5 (2007-01-01).
I commend this article and indeed the Ringholm site for a careful browse and review.
There are all sorts of lessons for Australia I believe here. The approach to security and privacy I found was especially pragmatic and robust.
I find it fascinating that the Dutch have committed so robustly to making HL7 V3.0 and CDA R2 work – despite it not being totally finalised – and seem to be having considerable success. This is encouraging news.
David.
The video describes AORTA which is the Dutch national infrastructure for the exchange of data between healthcare providers. The infrastructure specifications include a description of technical, organizational as well as implementation aspects. The focus of this program is to facilitate the realization of a national "continuity of care" oriented EHR. AORTA uses HL7 version 3 messages and documents as its core mechanism for information exchange.
Depending on your media preference you have a choice of formats.
AORTA introductory video (in English, 10 minutes),
http://www.uzi-register.nl/media/EMD_WDH_EN_256K.wmv (Windows Media file)
or
http://www.uzi-register.nl/media/EMD_WDH_EN_H264%20.mov (Apple Quicktime).
Vastly more information and detail on the project can be found at:
http://www.ringholm.de/docs/00980_en.htm
The author is René Spronk - Sr.Consultant, Ringholm GmbH
The current document status: Draft, version 0.5 (2007-01-01).
I commend this article and indeed the Ringholm site for a careful browse and review.
There are all sorts of lessons for Australia I believe here. The approach to security and privacy I found was especially pragmatic and robust.
I find it fascinating that the Dutch have committed so robustly to making HL7 V3.0 and CDA R2 work – despite it not being totally finalised – and seem to be having considerable success. This is encouraging news.
David.
Wednesday, March 07, 2007
Why the NEHTA Clinical Data Specifications Will Go Nowhere.
In early 2002 an organisation called the National Infostructure Development (NID) was funded to develop the information infrastructure that would be required as part of an implementation of the then planned HealthConnect. A key component was the Clinical Information Project (CIP).
The CIP focus was the clinical information content of shared EHRs for HealthConnect and the broader EHR agenda. The clinical information content relates to information that needs to be captured, stored and viewed to support the HealthConnect objective of improved delivery of health care and better quality of care.
Because the developmental focus of HealthConnect as a whole was based on the concept of event summaries, which were to make up the Shared EHR, the focus of the CIP was on the development of forms together with information content and definitions suitable for discharge summaries, referrals, result information and so on (the so called 'high priority' forms).
Efforts in this area continued when NEHTA took over responsibility for the CIP – since renamed a couple of times and, now seen as part of the Clinical Communications component of NEHTA's work. Recently (in December, 2006 and in February) we witnessed the release of two 500 page documents outlining the information structure and content of discharge summaries and specialist referrals.
What are we to make of these documents and how are they to be used?
_________________________________
In their introductory document the authors say:-
“NEHTA has released specifications to standardise the content of electronic referrals across Australia. This work also makes possible the development of improved decision support systems, which will be able to make use of the information in electronic versions of clinical documents (such as referrals) to assist healthcare practitioners make better decisions; and is an important step towards realising shared electronic health records.”
And they also say:-
“A Comprehensive Specification
It is important to understand the philosophy behind specifying referral content as comprehensively as appears in this specification. The specification needs to be comprehensive to capture as much information as required for the recipient to understand the patient's condition as fully as possible. However, it is quite clear that any one referral sent by a healthcare practitioner is unlikely to require the full suite of details embodied in the specification. In developing the referral specification, NEHTA has considered:
• - how prescriptive the referral template should be, in terms of:
o structure;
o comprehensiveness; and
o the terminology used;
• - the burden imposed on clinicians creating and receiving referrals; and
•- the burden on clinical information systems to capture, send and/or receive and process structured information.
Therefore, while the specification is prescriptive with respect to structure, information richness, and terminology, it is not prescriptive about which information should be sent under what circumstances. It is important to note that the specification was also designed for use within clinical information systems to reduce the burden of data entry for the referring healthcare provider, and the subsequent data interpretation, storage and manipulation by the referred-to provider.
The specification and included samples therefore indicate the richness of information that can be expressed, sent and ultimately imported into clinical information systems and shared electronic health records. The specification should not be interpreted as the set of information that must be sent, irrespective of the condition of the patient and the purpose of the referral.
Implementation Considerations
The establishment of clinical information systems that can interoperate regarding the transmission and computer interpretation of referrals (and other documents) is an evolutionary process. NEHTA anticipates that, in the first instance, the health community will review the GP and Specialist/Critical Care Referral Content Specification to become familiar with the content and intention of the specification, and plan to implement elements of the specification where possible within planned system upgrades.
Once the additional elements required by interoperable systems become available, the systems that have incorporated the specification will be able to quickly transition to interoperability. The key additional elements are outlined below.”
____________________________________
The document then goes on to cite SNOMED CT, HL7 V2.x and provider and patient identification.
I must say it takes some special form of arrogance to publish a set of specifications such as this without any reference to, or suggestion of, even the simplest of trial implementations, or ‘proof of concept and viability’, or any of the tools that are obviously required to make any sense or use of the material.
I am sure any system provider offered this specification would say: “Where in the world is something of this structure and complexity working and how much are you going to pay me to be your trial horse?”
Comments such as “NEHTA anticipates that, in the first instance, the health community will review the GP and Specialist/Critical Care Referral Content Specification to become familiar with the content and intention of the specification, and plan to implement elements of the specification where possible within planned system upgrades.” provide no assurance any of this is going anywhere in the foreseeable future – and leads to the inevitable question “Why should I spend anything on all this until it is clear that others are?”.
The other obvious problem is that NEHTA says that one does not need to do a comprehensive implementation of this specification but provides no roadmap to guide development and implementation priorities. Unless this is provided this looks like it’s pretty much an 'all or none' in terms of what is needed to begin developing system specifications. And the “all” is a huge project I would suggest, especially as the specification seems to only exist as an untested MS Word document at present!
The last major issue is that nowhere in the documentation is there any mention of how interoperation, if ever attempted, will be certified and provide a robust guarantee of accuracy, reliability, future maintenance and safety. If you offer a specification of this nature for use you take on the obligation to maintain and certify compliance with the specifications that you produce in perpetuity. Plans in this area simply do not exist as far as I can tell.
Slipping back to reality for a moment, the facts are these:
1. A national HealthConnect project, as originally envisaged, seems to have a very low probability of actually ever being implemented, even though NEHTA says it is still being worked on. The most obvious reason for this is that the costs of such a project (almost certainly billions of dollars) are not likely to easily be provided by Government – despite a compelling business case to make major investments in the e-Health space.
2. The world has moved on to more pragmatic international standards with experts and implementers on both sides of the Atlantic seeking simpler and more practical implementable approaches for deployment of interoperable systems. In the US the Continuity of Care Document (CCD) is emerging (deploying features of HL7, CDA R2 and ASTM CCR) as a credible standard and in the UK work has been undertaken to reduce the information content on the NHS Spine down to the minimum possible.
3. Without a guarantee of major investment in these specifications no vendor will invest to develop compliance. Attempts at mandating such specifications are likewise doomed as large vendors will simply say 'you set up the certification mechanisms so compliance can be verified and you pay us all our costs at time and material rates and we will develop what you require!” Meanwhile, small vendors will probably be put out of business if they attempt to address the complexity inherent in the specifications.
4. Unless the specification is implemented as a whole how are partially compliant systems to ‘understand’ what they are being sent? There are also versioning and maintenance issues that will emerge over time that are not addressed as best I can see. What is likely to happen as new versions of this specification are developed or new terminology is implemented. All of a sudden interoperation between old and new versions will become much more problematic. OpenEHR and its predecessor designs have devoted vast effort to addressing such matters. It is not clear the same is true with this work.
It seems clear that as of now, NEHTA would be far better off working with HL7 to spend whatever limited resources are available to assist with and influence the CCD and make sure it is suitable for Australia rather than continuing with what is an ill-considered, go it alone, and now past its time, local initiative. That way, more local skills in support of a global standard and its implementation would be developed in Australia. This in turn would enable Australia to maintain a place at the 'top table' of standards developers, and ensure that it can draw upon various sources of implementation capabilities and resources internationally.
Unless NEHTA is prepared to fund a range of genuine ‘proof of concept’ implementations of its specifications (to confirm their functionality, utility, viability and technical correctness) this is all going to be a waste of time and money. Even if NEHTA does decide to take that path the likelihood of eventual adoption by the Australian Health IT community would have to be rated as unlikely at best.
David.
The CIP focus was the clinical information content of shared EHRs for HealthConnect and the broader EHR agenda. The clinical information content relates to information that needs to be captured, stored and viewed to support the HealthConnect objective of improved delivery of health care and better quality of care.
Because the developmental focus of HealthConnect as a whole was based on the concept of event summaries, which were to make up the Shared EHR, the focus of the CIP was on the development of forms together with information content and definitions suitable for discharge summaries, referrals, result information and so on (the so called 'high priority' forms).
Efforts in this area continued when NEHTA took over responsibility for the CIP – since renamed a couple of times and, now seen as part of the Clinical Communications component of NEHTA's work. Recently (in December, 2006 and in February) we witnessed the release of two 500 page documents outlining the information structure and content of discharge summaries and specialist referrals.
What are we to make of these documents and how are they to be used?
_________________________________
In their introductory document the authors say:-
“NEHTA has released specifications to standardise the content of electronic referrals across Australia. This work also makes possible the development of improved decision support systems, which will be able to make use of the information in electronic versions of clinical documents (such as referrals) to assist healthcare practitioners make better decisions; and is an important step towards realising shared electronic health records.”
And they also say:-
“A Comprehensive Specification
It is important to understand the philosophy behind specifying referral content as comprehensively as appears in this specification. The specification needs to be comprehensive to capture as much information as required for the recipient to understand the patient's condition as fully as possible. However, it is quite clear that any one referral sent by a healthcare practitioner is unlikely to require the full suite of details embodied in the specification. In developing the referral specification, NEHTA has considered:
• - how prescriptive the referral template should be, in terms of:
o structure;
o comprehensiveness; and
o the terminology used;
• - the burden imposed on clinicians creating and receiving referrals; and
•- the burden on clinical information systems to capture, send and/or receive and process structured information.
Therefore, while the specification is prescriptive with respect to structure, information richness, and terminology, it is not prescriptive about which information should be sent under what circumstances. It is important to note that the specification was also designed for use within clinical information systems to reduce the burden of data entry for the referring healthcare provider, and the subsequent data interpretation, storage and manipulation by the referred-to provider.
The specification and included samples therefore indicate the richness of information that can be expressed, sent and ultimately imported into clinical information systems and shared electronic health records. The specification should not be interpreted as the set of information that must be sent, irrespective of the condition of the patient and the purpose of the referral.
Implementation Considerations
The establishment of clinical information systems that can interoperate regarding the transmission and computer interpretation of referrals (and other documents) is an evolutionary process. NEHTA anticipates that, in the first instance, the health community will review the GP and Specialist/Critical Care Referral Content Specification to become familiar with the content and intention of the specification, and plan to implement elements of the specification where possible within planned system upgrades.
Once the additional elements required by interoperable systems become available, the systems that have incorporated the specification will be able to quickly transition to interoperability. The key additional elements are outlined below.”
____________________________________
The document then goes on to cite SNOMED CT, HL7 V2.x and provider and patient identification.
I must say it takes some special form of arrogance to publish a set of specifications such as this without any reference to, or suggestion of, even the simplest of trial implementations, or ‘proof of concept and viability’, or any of the tools that are obviously required to make any sense or use of the material.
I am sure any system provider offered this specification would say: “Where in the world is something of this structure and complexity working and how much are you going to pay me to be your trial horse?”
Comments such as “NEHTA anticipates that, in the first instance, the health community will review the GP and Specialist/Critical Care Referral Content Specification to become familiar with the content and intention of the specification, and plan to implement elements of the specification where possible within planned system upgrades.” provide no assurance any of this is going anywhere in the foreseeable future – and leads to the inevitable question “Why should I spend anything on all this until it is clear that others are?”.
The other obvious problem is that NEHTA says that one does not need to do a comprehensive implementation of this specification but provides no roadmap to guide development and implementation priorities. Unless this is provided this looks like it’s pretty much an 'all or none' in terms of what is needed to begin developing system specifications. And the “all” is a huge project I would suggest, especially as the specification seems to only exist as an untested MS Word document at present!
The last major issue is that nowhere in the documentation is there any mention of how interoperation, if ever attempted, will be certified and provide a robust guarantee of accuracy, reliability, future maintenance and safety. If you offer a specification of this nature for use you take on the obligation to maintain and certify compliance with the specifications that you produce in perpetuity. Plans in this area simply do not exist as far as I can tell.
Slipping back to reality for a moment, the facts are these:
1. A national HealthConnect project, as originally envisaged, seems to have a very low probability of actually ever being implemented, even though NEHTA says it is still being worked on. The most obvious reason for this is that the costs of such a project (almost certainly billions of dollars) are not likely to easily be provided by Government – despite a compelling business case to make major investments in the e-Health space.
2. The world has moved on to more pragmatic international standards with experts and implementers on both sides of the Atlantic seeking simpler and more practical implementable approaches for deployment of interoperable systems. In the US the Continuity of Care Document (CCD) is emerging (deploying features of HL7, CDA R2 and ASTM CCR) as a credible standard and in the UK work has been undertaken to reduce the information content on the NHS Spine down to the minimum possible.
3. Without a guarantee of major investment in these specifications no vendor will invest to develop compliance. Attempts at mandating such specifications are likewise doomed as large vendors will simply say 'you set up the certification mechanisms so compliance can be verified and you pay us all our costs at time and material rates and we will develop what you require!” Meanwhile, small vendors will probably be put out of business if they attempt to address the complexity inherent in the specifications.
4. Unless the specification is implemented as a whole how are partially compliant systems to ‘understand’ what they are being sent? There are also versioning and maintenance issues that will emerge over time that are not addressed as best I can see. What is likely to happen as new versions of this specification are developed or new terminology is implemented. All of a sudden interoperation between old and new versions will become much more problematic. OpenEHR and its predecessor designs have devoted vast effort to addressing such matters. It is not clear the same is true with this work.
It seems clear that as of now, NEHTA would be far better off working with HL7 to spend whatever limited resources are available to assist with and influence the CCD and make sure it is suitable for Australia rather than continuing with what is an ill-considered, go it alone, and now past its time, local initiative. That way, more local skills in support of a global standard and its implementation would be developed in Australia. This in turn would enable Australia to maintain a place at the 'top table' of standards developers, and ensure that it can draw upon various sources of implementation capabilities and resources internationally.
Unless NEHTA is prepared to fund a range of genuine ‘proof of concept’ implementations of its specifications (to confirm their functionality, utility, viability and technical correctness) this is all going to be a waste of time and money. Even if NEHTA does decide to take that path the likelihood of eventual adoption by the Australian Health IT community would have to be rated as unlikely at best.
David.
Monday, March 05, 2007
Why Should Commonwealth e-Health Executives be having Sleepless Nights?
NEHTA gave a presentation at the 9th Annual AFR Health Congress last week. This presentation confirms my worst fears. From the presentation it is now clear that fantasy and wishful thinking have replaced any rationality that may have once been evident.
I am now able to confidently declare the NEHTA experiment to be a dangerous, destructive (of many committed professionals in the area) and expensive failure, and I am confident it will soon become a 'career limiting' blot on the resumes of many of those involved.
It cannot be too long before the Minister is forced to intervene and try and rescue some of the worthwhile cargo from the sinking ship. How can I be sure? Let me provide the evidence.
Let's start with the title of the presentation “Accelerating e-Health in Australia”. This is hardly true – we are told in the presentation that the time frame for benefits realisation is 10 years and that current implementation plans for the most basic of services will take at least 3-4 years from now.
NEHTA claims to be managing four major projects. Let us consider each in turn
1. Benefits – Seeking to identify the greatest benefits for least cost, in the shortest time, with least risk
Great words but from where will the benefits come?
We are told the benefits will come from (presumed enhancements in):
“Safety –reduced incidence & severity of injury
Effectiveness –avoiding under-use, misuse & over-use
Patient-centeredness -supports continuity of care & patient self-management
Timelines –reducing queues, overcrowding, harmful delays
Efficiency –avoiding waste in equipment, supplies, resources
Equity –in location, socioeconomic status, ethnicity & gender”
What we are not told is ‘the how’. What systems, doing what, used by whom, paid for by whom, with what functionality and so on will yield this bounty?
The benefits are said to be coming from improvements in pharmacy, hospital and general practice processes, messaging efficiency and clinical decision support. How much more generic could one be. Of course if you put quality systems in to support these activities there will probably be benefits.
Work like this was done over five years ago in the US, UK and Canada and it was done better and provided much more detail regarding the systems required, the dependencies and the scale of investment required.
Furthermore the brightly coloured graphs provided are completely meaningless as they lack any scales, values or axes. I would suggest that benefits claimed without any quantification (or even estimates) are hardly real believable benefits. Where, one asks, is the information to support these slides – secret I suppose yet again – or does it actually exist?
Without this information what we have is a claim for benefits derived from systems we don't presently have and at present do not seem to have any plans (or funds) to purchase. It is fantastic – in the true sense of that word.
The two reasons to undertake benefits studies are to justify investment in Health IT and to assist in the management of benefits realisation during system implementation. What NEHTA provides is wholly inadequate to either task. Without much more detail one is left with the distinct impression no detail exists when it is clear a compelling case for investment can be made and should be made but this must be backed up by substance and free of the motherhood as provided here.
2. Identifiers -Uniquely identifying individuals and healthcare providers across Australia
This project has been overtaken by events. With the decision to implement the Human Services Access Card in April 2006, there should have been an immediate review by NEHTA of the plans earlier (February 2006) for identification management systems, to understand how the Access Card proposal could be best melded with the need for individual identification in the e-health environment before too much time and money were wasted.
This has not happened and any relationship between the two projects is disavowed by NEHTA. This is just silly! The facts are:
(a) The Access Card is intended to identify Health Sector Clients for Medicare Benefits and NEHTA is planning to use Medicare ID data for its Identifier.
(b) Both Projects are allocating citizens an ID number and establishing a data-base of basic demographic information.
(c) The NEHTA identifier will be allocated to citizens without their knowledge or consent and if errors occur the citizen will not have access to correct and view the information held.
(d) The NEHTA identifier is likely to be both less 'robust' and more potentially privacy invasive due to its covert existence.
I suspect NEHTA has been given some money and really wants to spend it – and that the ultimate casualty will be a very angry public when it is realised how they are all essentially being secretly numbered while at the same time having to obtain an access card. Again this seems to me to be 'career limiting' for the responsible bureaucrats if not remedied.
3. Terminologies -Exchanging clinical information electronically, using a common language with consistent terms, descriptions and formats.
This is important work but it is not being delivered at the pace NEHTA promised. It is clear the Australian Medicines Terminology extension of SNOMED CT (the national clinical terminology) is significantly delayed (it was promised for January 2007) and the work released on pathology terminology is, by NEHTA's own admission, not ready for implementation.
Without attributing any blame it is also clear that negotiations to set up the international Standards Development Organisation to manage SNOMED CT is also taking longer than expected. (It was meant to be done late in 2006).
4. Shared EHR (SEHR) -Designing a national system of shared electronic health records for authorised practitioners and consumers.
Work in this area would seem to have slowed to a dawdle with only a two page statement of intent issued in the last twelve months (in August 2006). I suspect those responsible have recognised that a national SEHR is much bigger and more complex than they ever envisaged when they were given the abandoned carcass of the HealthConnect project to resurrect in late 2004.
It is worth noting that the time frame for the review of SEHR Standards was twelve to eighteen months after the development of the original report on February 2006. Since that time very little progress seems to have been made with EN13606 (which is still not approved) and NEHTA has apparently declined the opportunity to further develop HL7 V2.x messaging templates as an interim clinical content transfer approach. Meanwhile there has been significant progress on the HL7 Services front and on CDA R2, CCR and CCD making much of the work done in late 2005 for the report obsolete and urgently in need of re-assessment.
5. The fifth project, which is only partially mentioned in the presentation is the development of Secure Messaging for the Health System and the associated Clinical Data Standards for a number of key messages (Discharge Summaries, Referrals etc).
Here we have the secure message providers (HealthLink, Medical Objects, Argus Connect, Promedicus.net, and others) essentially being forced into going their own ways – based on HL7 V2.x or PIT – and the Clinical Data Standards Project continuing on with work based on HealthConnect’s requirements of 2004/5 whilst essentially ignoring the now internationally standardised alternatives for practical health information sharing. It just gets sillier and more wasteful by the month.
What is to be done?
I think the first thing that is needed are the facts. For that reason, as I have suggested previously, I believe we need a professionally conducted enquiry into e-Health for the last decade to get out in the open all the secret reports and make transparent just what has gone well and what has gone badly. The enquiry should also include a thorough audit of the status quo in regards to NEHTA's activities, work-plans, project management structure(s), budgeting and financial controls. This is particularly important in order to see behind the corporate veil which NEHTA has constructed that enables it to avoid being subjected to the rigours of public accountability.
This enquiry would be like the independent enquires conducted in the UK by the Audit Office or in the US by the Government Accountability Office. It would be hard to argue that such a review is not warranted – even on the basis of the obvious facts that the initial vision of 2000/2001 has not been anywhere near delivered some six years later and to ask why.
Another reason an enquiry is needed is that I would argue we have never tried a real model of an AHIC (clinician and expert led) governing a technical execution arm. This is what I took the Boston Consulting Group report as aiming to set up. What happened is that the Government set up the technology component with largely only technology leadership and then moved it away from direct DoHA control and placed control with a non-expert (in Health IT) board.
To show how far implementation has slipped one only has to return to the April 2004 Boston Consulting Group Report. Three years following the report it was intended that:
“ Connectivity building blocks largely in place
- 'Critical mass' of new interoperable clinical and administrative systems
- Key standards agreed and implemented by authoritative body
- Significant broad band/required infrastructure roll-out across country
- High-system users aware of consent issues and electronic benefits
- Significant numbers of providers have experience of clinical messaging and order entry applications
- Expanded information available for research, policy purposes and administrative uses.”
How close are we now to this happy state? Look closely at what was recommended and compare with what we presently have.
Source: BCG April 2004.
It is only when armed with independently acquired facts that a really rational and workable forward plan can be developed.
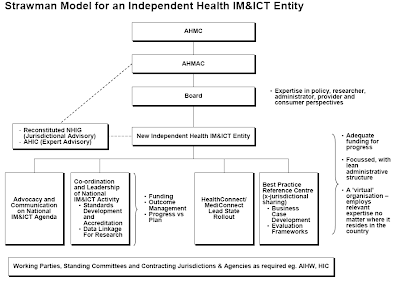
For what its worth I believe that essentially the technologically driven 'tail' needs to stop wagging the health sector 'dog'. If the revised Australian Health Information Council (AHIC) had executive authority, a relevant mix of Health and Health IT experts and appropriate funds, it would be the ideal entity to take direct control of the NEHTA agenda and work plan. As this does not seem to be the case an alternative approach is required.
As I see it, the problem is that there really needs to be a holistic strategic and low level integrated approach i.e. all the aspects from identifying the problems, finding approaches and solutions, then doing the actual work [differentiating what should be done by the market and by Government(s)] in a co-ordinated way at the technical, standards and strategic levels.
Having a non-strategic 'tech shop', which operates in a strategic vacuum, and which claims strategic responsibility for Australian E-Health is a real problem - they (the Council of Australian Governments) have created a strategically 'headless chook' and we are now seeing the results.
So NEHTA has become the answer to a question that was not properly framed by the Boston Consulting Group - and this has led, combined with the dismemberment of AHIC, to the dysfunction we now see.
The reason we have gone down this path is that the business case, which should have been acceptable to Government to initiate a reasonable level of investment, was never done (as it was in the US, UK and Canada) and so, without any real investment co-ordination and scale, nothing has happened. And nothing will happen until that changes and this joke of an effort which masquerades as a business case from NEHTA (see the two colour slides) is redone to really get us there. There is good evidence available and this effort does not exploit it at all.
NEHTA does not see the gap between what it is doing and the need to have a real, achievable and immediate impact on health services (which is, I believe, huge).
We need a fully funded strategic e-Health entity which has the role of driving NEHTA down a more health sector focussed role and setting priorities for the whole sector - with a mix of vendor and home developed solutions and an openness to working with industry, academia, clinicians, and others.
It might be possible to add to NEHTA a strategy unit and a decent health sector liaison unit and change the CEO to someone more fitted to the role. The present leadership have shown an absence of strategic nous and health sector understanding and should only continue in operational delivery rather than strategic planning roles.
We also need to get real political accountability back - so heat can be felt and reacted to for the betterment of all! NEHTA really needs to be back under normal public sector management and accountability.
At HIMMS 07 (a few days ago) we had NEHTA deliver a presentation entitled “Successful E - Health Transitions: Australia's E- Health Initiatives”. Given what NEHTA has failed to deliver over the last three years or so, I would hate to know what failure looked like if this is success!
A major strategic change is needed, based on real independent evidence of what is working and what is not, and it can't come soon enough. The bureaucrats who are fond of their jobs really need to get a reality check, and initiate major change of the sort I outline, or suffer a pretty nasty fate once the Minister realises just how badly things have really gone, how many lives have been damaged or worse, and how much money has been wasted.
David.
I am now able to confidently declare the NEHTA experiment to be a dangerous, destructive (of many committed professionals in the area) and expensive failure, and I am confident it will soon become a 'career limiting' blot on the resumes of many of those involved.
It cannot be too long before the Minister is forced to intervene and try and rescue some of the worthwhile cargo from the sinking ship. How can I be sure? Let me provide the evidence.
Let's start with the title of the presentation “Accelerating e-Health in Australia”. This is hardly true – we are told in the presentation that the time frame for benefits realisation is 10 years and that current implementation plans for the most basic of services will take at least 3-4 years from now.
NEHTA claims to be managing four major projects. Let us consider each in turn
1. Benefits – Seeking to identify the greatest benefits for least cost, in the shortest time, with least risk
Great words but from where will the benefits come?
We are told the benefits will come from (presumed enhancements in):
“Safety –reduced incidence & severity of injury
Effectiveness –avoiding under-use, misuse & over-use
Patient-centeredness -supports continuity of care & patient self-management
Timelines –reducing queues, overcrowding, harmful delays
Efficiency –avoiding waste in equipment, supplies, resources
Equity –in location, socioeconomic status, ethnicity & gender”
What we are not told is ‘the how’. What systems, doing what, used by whom, paid for by whom, with what functionality and so on will yield this bounty?
The benefits are said to be coming from improvements in pharmacy, hospital and general practice processes, messaging efficiency and clinical decision support. How much more generic could one be. Of course if you put quality systems in to support these activities there will probably be benefits.
Work like this was done over five years ago in the US, UK and Canada and it was done better and provided much more detail regarding the systems required, the dependencies and the scale of investment required.
Furthermore the brightly coloured graphs provided are completely meaningless as they lack any scales, values or axes. I would suggest that benefits claimed without any quantification (or even estimates) are hardly real believable benefits. Where, one asks, is the information to support these slides – secret I suppose yet again – or does it actually exist?
Without this information what we have is a claim for benefits derived from systems we don't presently have and at present do not seem to have any plans (or funds) to purchase. It is fantastic – in the true sense of that word.
The two reasons to undertake benefits studies are to justify investment in Health IT and to assist in the management of benefits realisation during system implementation. What NEHTA provides is wholly inadequate to either task. Without much more detail one is left with the distinct impression no detail exists when it is clear a compelling case for investment can be made and should be made but this must be backed up by substance and free of the motherhood as provided here.
2. Identifiers -Uniquely identifying individuals and healthcare providers across Australia
This project has been overtaken by events. With the decision to implement the Human Services Access Card in April 2006, there should have been an immediate review by NEHTA of the plans earlier (February 2006) for identification management systems, to understand how the Access Card proposal could be best melded with the need for individual identification in the e-health environment before too much time and money were wasted.
This has not happened and any relationship between the two projects is disavowed by NEHTA. This is just silly! The facts are:
(a) The Access Card is intended to identify Health Sector Clients for Medicare Benefits and NEHTA is planning to use Medicare ID data for its Identifier.
(b) Both Projects are allocating citizens an ID number and establishing a data-base of basic demographic information.
(c) The NEHTA identifier will be allocated to citizens without their knowledge or consent and if errors occur the citizen will not have access to correct and view the information held.
(d) The NEHTA identifier is likely to be both less 'robust' and more potentially privacy invasive due to its covert existence.
I suspect NEHTA has been given some money and really wants to spend it – and that the ultimate casualty will be a very angry public when it is realised how they are all essentially being secretly numbered while at the same time having to obtain an access card. Again this seems to me to be 'career limiting' for the responsible bureaucrats if not remedied.
3. Terminologies -Exchanging clinical information electronically, using a common language with consistent terms, descriptions and formats.
This is important work but it is not being delivered at the pace NEHTA promised. It is clear the Australian Medicines Terminology extension of SNOMED CT (the national clinical terminology) is significantly delayed (it was promised for January 2007) and the work released on pathology terminology is, by NEHTA's own admission, not ready for implementation.
Without attributing any blame it is also clear that negotiations to set up the international Standards Development Organisation to manage SNOMED CT is also taking longer than expected. (It was meant to be done late in 2006).
4. Shared EHR (SEHR) -Designing a national system of shared electronic health records for authorised practitioners and consumers.
Work in this area would seem to have slowed to a dawdle with only a two page statement of intent issued in the last twelve months (in August 2006). I suspect those responsible have recognised that a national SEHR is much bigger and more complex than they ever envisaged when they were given the abandoned carcass of the HealthConnect project to resurrect in late 2004.
It is worth noting that the time frame for the review of SEHR Standards was twelve to eighteen months after the development of the original report on February 2006. Since that time very little progress seems to have been made with EN13606 (which is still not approved) and NEHTA has apparently declined the opportunity to further develop HL7 V2.x messaging templates as an interim clinical content transfer approach. Meanwhile there has been significant progress on the HL7 Services front and on CDA R2, CCR and CCD making much of the work done in late 2005 for the report obsolete and urgently in need of re-assessment.
5. The fifth project, which is only partially mentioned in the presentation is the development of Secure Messaging for the Health System and the associated Clinical Data Standards for a number of key messages (Discharge Summaries, Referrals etc).
Here we have the secure message providers (HealthLink, Medical Objects, Argus Connect, Promedicus.net, and others) essentially being forced into going their own ways – based on HL7 V2.x or PIT – and the Clinical Data Standards Project continuing on with work based on HealthConnect’s requirements of 2004/5 whilst essentially ignoring the now internationally standardised alternatives for practical health information sharing. It just gets sillier and more wasteful by the month.
What is to be done?
I think the first thing that is needed are the facts. For that reason, as I have suggested previously, I believe we need a professionally conducted enquiry into e-Health for the last decade to get out in the open all the secret reports and make transparent just what has gone well and what has gone badly. The enquiry should also include a thorough audit of the status quo in regards to NEHTA's activities, work-plans, project management structure(s), budgeting and financial controls. This is particularly important in order to see behind the corporate veil which NEHTA has constructed that enables it to avoid being subjected to the rigours of public accountability.
This enquiry would be like the independent enquires conducted in the UK by the Audit Office or in the US by the Government Accountability Office. It would be hard to argue that such a review is not warranted – even on the basis of the obvious facts that the initial vision of 2000/2001 has not been anywhere near delivered some six years later and to ask why.
Another reason an enquiry is needed is that I would argue we have never tried a real model of an AHIC (clinician and expert led) governing a technical execution arm. This is what I took the Boston Consulting Group report as aiming to set up. What happened is that the Government set up the technology component with largely only technology leadership and then moved it away from direct DoHA control and placed control with a non-expert (in Health IT) board.
To show how far implementation has slipped one only has to return to the April 2004 Boston Consulting Group Report. Three years following the report it was intended that:
“ Connectivity building blocks largely in place
- 'Critical mass' of new interoperable clinical and administrative systems
- Key standards agreed and implemented by authoritative body
- Significant broad band/required infrastructure roll-out across country
- High-system users aware of consent issues and electronic benefits
- Significant numbers of providers have experience of clinical messaging and order entry applications
- Expanded information available for research, policy purposes and administrative uses.”
How close are we now to this happy state? Look closely at what was recommended and compare with what we presently have.
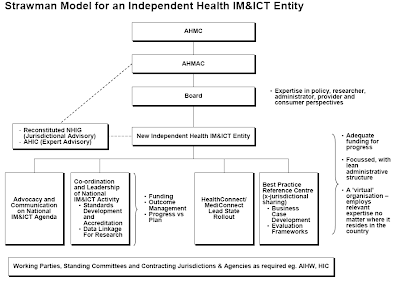
Source: BCG April 2004.
It is only when armed with independently acquired facts that a really rational and workable forward plan can be developed.
For what its worth I believe that essentially the technologically driven 'tail' needs to stop wagging the health sector 'dog'. If the revised Australian Health Information Council (AHIC) had executive authority, a relevant mix of Health and Health IT experts and appropriate funds, it would be the ideal entity to take direct control of the NEHTA agenda and work plan. As this does not seem to be the case an alternative approach is required.
As I see it, the problem is that there really needs to be a holistic strategic and low level integrated approach i.e. all the aspects from identifying the problems, finding approaches and solutions, then doing the actual work [differentiating what should be done by the market and by Government(s)] in a co-ordinated way at the technical, standards and strategic levels.
Having a non-strategic 'tech shop', which operates in a strategic vacuum, and which claims strategic responsibility for Australian E-Health is a real problem - they (the Council of Australian Governments) have created a strategically 'headless chook' and we are now seeing the results.
So NEHTA has become the answer to a question that was not properly framed by the Boston Consulting Group - and this has led, combined with the dismemberment of AHIC, to the dysfunction we now see.
The reason we have gone down this path is that the business case, which should have been acceptable to Government to initiate a reasonable level of investment, was never done (as it was in the US, UK and Canada) and so, without any real investment co-ordination and scale, nothing has happened. And nothing will happen until that changes and this joke of an effort which masquerades as a business case from NEHTA (see the two colour slides) is redone to really get us there. There is good evidence available and this effort does not exploit it at all.
NEHTA does not see the gap between what it is doing and the need to have a real, achievable and immediate impact on health services (which is, I believe, huge).
We need a fully funded strategic e-Health entity which has the role of driving NEHTA down a more health sector focussed role and setting priorities for the whole sector - with a mix of vendor and home developed solutions and an openness to working with industry, academia, clinicians, and others.
It might be possible to add to NEHTA a strategy unit and a decent health sector liaison unit and change the CEO to someone more fitted to the role. The present leadership have shown an absence of strategic nous and health sector understanding and should only continue in operational delivery rather than strategic planning roles.
We also need to get real political accountability back - so heat can be felt and reacted to for the betterment of all! NEHTA really needs to be back under normal public sector management and accountability.
At HIMMS 07 (a few days ago) we had NEHTA deliver a presentation entitled “Successful E - Health Transitions: Australia's E- Health Initiatives”. Given what NEHTA has failed to deliver over the last three years or so, I would hate to know what failure looked like if this is success!
A major strategic change is needed, based on real independent evidence of what is working and what is not, and it can't come soon enough. The bureaucrats who are fond of their jobs really need to get a reality check, and initiate major change of the sort I outline, or suffer a pretty nasty fate once the Minister realises just how badly things have really gone, how many lives have been damaged or worse, and how much money has been wasted.
David.
Sunday, March 04, 2007
An Invaluable Reference on Health IT Value
Just a very short post to make sure everyone is aware of this invaluable site.
It is titled:
The case for IT in healthcare – supporting the patient safety agenda
It contains links and summaries of a large number of reports that have shown a clear case for using IT in healthcare to bring safety benefits for patients.
This is the case we should be making to the Australian Government.
The URL is:
http://www.connectingforhealth.nhs.uk/about/case/the-case-for-it-in-healthcare
Enjoy browsing and use the material to convince others of the importance and value of pressing on with Health IT programs and initiatives.
While citing this site it occurs to me there are other invaluable sites that are well worth a browse.
My special favourites are:
For the USA.
http://www.ihealthbeat.org/
http://healthdatamanagement.com/
http://www.informatics-review.com/
http://www.govhealthit.com/
http://www.healthcareitnews.com/
For the UK.
http://www.informatics.nhs.uk/
http://www.e-health-insider.com/
And in Australia
http://australianit.news.com.au/topics/0,7202,news_ehealth_law,00.html
http://www.pulsemagazine.com.au/
For a link to many Health IT Blogs – this site is useful
http://www.hitsphere.com/
Enjoy browsing them all.
David.
It is titled:
The case for IT in healthcare – supporting the patient safety agenda
It contains links and summaries of a large number of reports that have shown a clear case for using IT in healthcare to bring safety benefits for patients.
This is the case we should be making to the Australian Government.
The URL is:
http://www.connectingforhealth.nhs.uk/about/case/the-case-for-it-in-healthcare
Enjoy browsing and use the material to convince others of the importance and value of pressing on with Health IT programs and initiatives.
While citing this site it occurs to me there are other invaluable sites that are well worth a browse.
My special favourites are:
For the USA.
http://www.ihealthbeat.org/
http://healthdatamanagement.com/
http://www.informatics-review.com/
http://www.govhealthit.com/
http://www.healthcareitnews.com/
For the UK.
http://www.informatics.nhs.uk/
http://www.e-health-insider.com/
And in Australia
http://australianit.news.com.au/topics/0,7202,news_ehealth_law,00.html
http://www.pulsemagazine.com.au/
For a link to many Health IT Blogs – this site is useful
http://www.hitsphere.com/
Enjoy browsing them all.
David.
AusHealthIT Turns One!
Well the blog is one year old on March 5, 2007. It now has one hundred and thirty eight entries and a regular readership that exceeds one hundred and fifty different individuals each time a new article is added.
The current top 10 most read articles are as follows:
1. Personal Health Information Privacy – The Elephant in the Room
2. Archetypically Stupid!
3. Electronic Prescribing – What is Needed to Move Forward?
4. NEHTA’s Annual Report – What We are Not Being Told.
5. Privacy Issues Related to the Proposed Access Card.
6. E-Mail Security and Clinical Practice.
7. E-Prescribing in Australia – Is there a New Plan?
8. How Did iSoft Get into So Much Trouble?
9. Clinical Research Information Now More Freely Available on the Internet.
10. AusHealthIT's First Guest Blogger Article.
Amazingly the different pages on the blog have now been viewed 13,333 times since I worked out how to set up a site counter in May, 2006.
The steady growth in feed subscribers has been encouraging and suggests that at least the blog is of interest and slightly controversial rather than being a total bore!
Feed Subscribers

What is there to learn from all this regarding the current state of and planned directions for E-Health in Australia? I take the following from the level of interest and the comments posted.
1. The topic of Health IT (e-health) is of interest to many more people than would initially be thought.
2. The topics of interest are – with a few exceptions – centred around the need for better policy in the area.
3. The themes of the blog in suggesting the need for a substantive National E-Health Strategy, Business Case and Implementation Plan and clarity around the importance of Health IT in the areas of patient safety and quality of care are supported.
4. The need to have sorted out a plan and then to ‘get on with it’ using proven and known technologies is totally un-controversial. There is widespread amazement in the E-Health community that the opportunity cost of doing nothing in the e-Health space is unrecognised. It is costing the community dearly in both lives and dollars.
5. Frustration with the lack of strategic clarity in the e-Health space is forcing development and implementation activity which is to be welcomed but which could be so much more effective and valuable if undertaken in a supportive, rational and co-ordinated framework.
6. There is widespread disappointment and frustration that NEHTA has focussed too much on the “E” and not enough on the “Health” leaving its efforts being seen as largely irrelevant to the Health Sector in general and increasingly the E-Health Community in particular. It is very important for NEHTA to be successful for E-Health in Australia to prosper and right now it does not seem to be heading in the right direction or listening to the E-Health Community very effectively.
I sense change is coming in this election year and also that Year 2 will be a very interesting one!
I would love comments on the above.
David.
The current top 10 most read articles are as follows:
1. Personal Health Information Privacy – The Elephant in the Room
2. Archetypically Stupid!
3. Electronic Prescribing – What is Needed to Move Forward?
4. NEHTA’s Annual Report – What We are Not Being Told.
5. Privacy Issues Related to the Proposed Access Card.
6. E-Mail Security and Clinical Practice.
7. E-Prescribing in Australia – Is there a New Plan?
8. How Did iSoft Get into So Much Trouble?
9. Clinical Research Information Now More Freely Available on the Internet.
10. AusHealthIT's First Guest Blogger Article.
Amazingly the different pages on the blog have now been viewed 13,333 times since I worked out how to set up a site counter in May, 2006.
The steady growth in feed subscribers has been encouraging and suggests that at least the blog is of interest and slightly controversial rather than being a total bore!
Feed Subscribers

What is there to learn from all this regarding the current state of and planned directions for E-Health in Australia? I take the following from the level of interest and the comments posted.
1. The topic of Health IT (e-health) is of interest to many more people than would initially be thought.
2. The topics of interest are – with a few exceptions – centred around the need for better policy in the area.
3. The themes of the blog in suggesting the need for a substantive National E-Health Strategy, Business Case and Implementation Plan and clarity around the importance of Health IT in the areas of patient safety and quality of care are supported.
4. The need to have sorted out a plan and then to ‘get on with it’ using proven and known technologies is totally un-controversial. There is widespread amazement in the E-Health community that the opportunity cost of doing nothing in the e-Health space is unrecognised. It is costing the community dearly in both lives and dollars.
5. Frustration with the lack of strategic clarity in the e-Health space is forcing development and implementation activity which is to be welcomed but which could be so much more effective and valuable if undertaken in a supportive, rational and co-ordinated framework.
6. There is widespread disappointment and frustration that NEHTA has focussed too much on the “E” and not enough on the “Health” leaving its efforts being seen as largely irrelevant to the Health Sector in general and increasingly the E-Health Community in particular. It is very important for NEHTA to be successful for E-Health in Australia to prosper and right now it does not seem to be heading in the right direction or listening to the E-Health Community very effectively.
I sense change is coming in this election year and also that Year 2 will be a very interesting one!
I would love comments on the above.
David.
Subscribe to:
Comments (Atom)