Just a short posting to provide a URL for a fascinating ten minute downloadable video that explains what the Dutch have been up to in e-Health over the last few years!
The video describes AORTA which is the Dutch national infrastructure for the exchange of data between healthcare providers. The infrastructure specifications include a description of technical, organizational as well as implementation aspects. The focus of this program is to facilitate the realization of a national "continuity of care" oriented EHR. AORTA uses HL7 version 3 messages and documents as its core mechanism for information exchange.
Depending on your media preference you have a choice of formats.
AORTA introductory video (in English, 10 minutes),
http://www.uzi-register.nl/media/EMD_WDH_EN_256K.wmv (Windows Media file)
or
http://www.uzi-register.nl/media/EMD_WDH_EN_H264%20.mov (Apple Quicktime).
Vastly more information and detail on the project can be found at:
http://www.ringholm.de/docs/00980_en.htm
The author is René Spronk - Sr.Consultant, Ringholm GmbH
The current document status: Draft, version 0.5 (2007-01-01).
I commend this article and indeed the Ringholm site for a careful browse and review.
There are all sorts of lessons for Australia I believe here. The approach to security and privacy I found was especially pragmatic and robust.
I find it fascinating that the Dutch have committed so robustly to making HL7 V3.0 and CDA R2 work – despite it not being totally finalised – and seem to be having considerable success. This is encouraging news.
David.
This blog is totally independent, unpaid and has only three major objectives.
The first is to inform readers of news and happenings in the e-Health domain, both here in Australia and world-wide.
The second is to provide commentary on e-Health in Australia and to foster improvement where I can.
The third is to encourage discussion of the matters raised in the blog so hopefully readers can get a balanced view of what is really happening and what successes are being achieved.
Quote Of The Year
Timeless Quotes - Sadly The Late Paul Shetler - "Its not Your Health Record it's a Government Record Of Your Health Information"
or
H. L. Mencken - "For every complex problem there is an answer that is clear, simple, and wrong."
Sunday, March 11, 2007
Wednesday, March 07, 2007
Why the NEHTA Clinical Data Specifications Will Go Nowhere.
In early 2002 an organisation called the National Infostructure Development (NID) was funded to develop the information infrastructure that would be required as part of an implementation of the then planned HealthConnect. A key component was the Clinical Information Project (CIP).
The CIP focus was the clinical information content of shared EHRs for HealthConnect and the broader EHR agenda. The clinical information content relates to information that needs to be captured, stored and viewed to support the HealthConnect objective of improved delivery of health care and better quality of care.
Because the developmental focus of HealthConnect as a whole was based on the concept of event summaries, which were to make up the Shared EHR, the focus of the CIP was on the development of forms together with information content and definitions suitable for discharge summaries, referrals, result information and so on (the so called 'high priority' forms).
Efforts in this area continued when NEHTA took over responsibility for the CIP – since renamed a couple of times and, now seen as part of the Clinical Communications component of NEHTA's work. Recently (in December, 2006 and in February) we witnessed the release of two 500 page documents outlining the information structure and content of discharge summaries and specialist referrals.
What are we to make of these documents and how are they to be used?
_________________________________
In their introductory document the authors say:-
“NEHTA has released specifications to standardise the content of electronic referrals across Australia. This work also makes possible the development of improved decision support systems, which will be able to make use of the information in electronic versions of clinical documents (such as referrals) to assist healthcare practitioners make better decisions; and is an important step towards realising shared electronic health records.”
And they also say:-
“A Comprehensive Specification
It is important to understand the philosophy behind specifying referral content as comprehensively as appears in this specification. The specification needs to be comprehensive to capture as much information as required for the recipient to understand the patient's condition as fully as possible. However, it is quite clear that any one referral sent by a healthcare practitioner is unlikely to require the full suite of details embodied in the specification. In developing the referral specification, NEHTA has considered:
• - how prescriptive the referral template should be, in terms of:
o structure;
o comprehensiveness; and
o the terminology used;
• - the burden imposed on clinicians creating and receiving referrals; and
•- the burden on clinical information systems to capture, send and/or receive and process structured information.
Therefore, while the specification is prescriptive with respect to structure, information richness, and terminology, it is not prescriptive about which information should be sent under what circumstances. It is important to note that the specification was also designed for use within clinical information systems to reduce the burden of data entry for the referring healthcare provider, and the subsequent data interpretation, storage and manipulation by the referred-to provider.
The specification and included samples therefore indicate the richness of information that can be expressed, sent and ultimately imported into clinical information systems and shared electronic health records. The specification should not be interpreted as the set of information that must be sent, irrespective of the condition of the patient and the purpose of the referral.
Implementation Considerations
The establishment of clinical information systems that can interoperate regarding the transmission and computer interpretation of referrals (and other documents) is an evolutionary process. NEHTA anticipates that, in the first instance, the health community will review the GP and Specialist/Critical Care Referral Content Specification to become familiar with the content and intention of the specification, and plan to implement elements of the specification where possible within planned system upgrades.
Once the additional elements required by interoperable systems become available, the systems that have incorporated the specification will be able to quickly transition to interoperability. The key additional elements are outlined below.”
____________________________________
The document then goes on to cite SNOMED CT, HL7 V2.x and provider and patient identification.
I must say it takes some special form of arrogance to publish a set of specifications such as this without any reference to, or suggestion of, even the simplest of trial implementations, or ‘proof of concept and viability’, or any of the tools that are obviously required to make any sense or use of the material.
I am sure any system provider offered this specification would say: “Where in the world is something of this structure and complexity working and how much are you going to pay me to be your trial horse?”
Comments such as “NEHTA anticipates that, in the first instance, the health community will review the GP and Specialist/Critical Care Referral Content Specification to become familiar with the content and intention of the specification, and plan to implement elements of the specification where possible within planned system upgrades.” provide no assurance any of this is going anywhere in the foreseeable future – and leads to the inevitable question “Why should I spend anything on all this until it is clear that others are?”.
The other obvious problem is that NEHTA says that one does not need to do a comprehensive implementation of this specification but provides no roadmap to guide development and implementation priorities. Unless this is provided this looks like it’s pretty much an 'all or none' in terms of what is needed to begin developing system specifications. And the “all” is a huge project I would suggest, especially as the specification seems to only exist as an untested MS Word document at present!
The last major issue is that nowhere in the documentation is there any mention of how interoperation, if ever attempted, will be certified and provide a robust guarantee of accuracy, reliability, future maintenance and safety. If you offer a specification of this nature for use you take on the obligation to maintain and certify compliance with the specifications that you produce in perpetuity. Plans in this area simply do not exist as far as I can tell.
Slipping back to reality for a moment, the facts are these:
1. A national HealthConnect project, as originally envisaged, seems to have a very low probability of actually ever being implemented, even though NEHTA says it is still being worked on. The most obvious reason for this is that the costs of such a project (almost certainly billions of dollars) are not likely to easily be provided by Government – despite a compelling business case to make major investments in the e-Health space.
2. The world has moved on to more pragmatic international standards with experts and implementers on both sides of the Atlantic seeking simpler and more practical implementable approaches for deployment of interoperable systems. In the US the Continuity of Care Document (CCD) is emerging (deploying features of HL7, CDA R2 and ASTM CCR) as a credible standard and in the UK work has been undertaken to reduce the information content on the NHS Spine down to the minimum possible.
3. Without a guarantee of major investment in these specifications no vendor will invest to develop compliance. Attempts at mandating such specifications are likewise doomed as large vendors will simply say 'you set up the certification mechanisms so compliance can be verified and you pay us all our costs at time and material rates and we will develop what you require!” Meanwhile, small vendors will probably be put out of business if they attempt to address the complexity inherent in the specifications.
4. Unless the specification is implemented as a whole how are partially compliant systems to ‘understand’ what they are being sent? There are also versioning and maintenance issues that will emerge over time that are not addressed as best I can see. What is likely to happen as new versions of this specification are developed or new terminology is implemented. All of a sudden interoperation between old and new versions will become much more problematic. OpenEHR and its predecessor designs have devoted vast effort to addressing such matters. It is not clear the same is true with this work.
It seems clear that as of now, NEHTA would be far better off working with HL7 to spend whatever limited resources are available to assist with and influence the CCD and make sure it is suitable for Australia rather than continuing with what is an ill-considered, go it alone, and now past its time, local initiative. That way, more local skills in support of a global standard and its implementation would be developed in Australia. This in turn would enable Australia to maintain a place at the 'top table' of standards developers, and ensure that it can draw upon various sources of implementation capabilities and resources internationally.
Unless NEHTA is prepared to fund a range of genuine ‘proof of concept’ implementations of its specifications (to confirm their functionality, utility, viability and technical correctness) this is all going to be a waste of time and money. Even if NEHTA does decide to take that path the likelihood of eventual adoption by the Australian Health IT community would have to be rated as unlikely at best.
David.
The CIP focus was the clinical information content of shared EHRs for HealthConnect and the broader EHR agenda. The clinical information content relates to information that needs to be captured, stored and viewed to support the HealthConnect objective of improved delivery of health care and better quality of care.
Because the developmental focus of HealthConnect as a whole was based on the concept of event summaries, which were to make up the Shared EHR, the focus of the CIP was on the development of forms together with information content and definitions suitable for discharge summaries, referrals, result information and so on (the so called 'high priority' forms).
Efforts in this area continued when NEHTA took over responsibility for the CIP – since renamed a couple of times and, now seen as part of the Clinical Communications component of NEHTA's work. Recently (in December, 2006 and in February) we witnessed the release of two 500 page documents outlining the information structure and content of discharge summaries and specialist referrals.
What are we to make of these documents and how are they to be used?
_________________________________
In their introductory document the authors say:-
“NEHTA has released specifications to standardise the content of electronic referrals across Australia. This work also makes possible the development of improved decision support systems, which will be able to make use of the information in electronic versions of clinical documents (such as referrals) to assist healthcare practitioners make better decisions; and is an important step towards realising shared electronic health records.”
And they also say:-
“A Comprehensive Specification
It is important to understand the philosophy behind specifying referral content as comprehensively as appears in this specification. The specification needs to be comprehensive to capture as much information as required for the recipient to understand the patient's condition as fully as possible. However, it is quite clear that any one referral sent by a healthcare practitioner is unlikely to require the full suite of details embodied in the specification. In developing the referral specification, NEHTA has considered:
• - how prescriptive the referral template should be, in terms of:
o structure;
o comprehensiveness; and
o the terminology used;
• - the burden imposed on clinicians creating and receiving referrals; and
•- the burden on clinical information systems to capture, send and/or receive and process structured information.
Therefore, while the specification is prescriptive with respect to structure, information richness, and terminology, it is not prescriptive about which information should be sent under what circumstances. It is important to note that the specification was also designed for use within clinical information systems to reduce the burden of data entry for the referring healthcare provider, and the subsequent data interpretation, storage and manipulation by the referred-to provider.
The specification and included samples therefore indicate the richness of information that can be expressed, sent and ultimately imported into clinical information systems and shared electronic health records. The specification should not be interpreted as the set of information that must be sent, irrespective of the condition of the patient and the purpose of the referral.
Implementation Considerations
The establishment of clinical information systems that can interoperate regarding the transmission and computer interpretation of referrals (and other documents) is an evolutionary process. NEHTA anticipates that, in the first instance, the health community will review the GP and Specialist/Critical Care Referral Content Specification to become familiar with the content and intention of the specification, and plan to implement elements of the specification where possible within planned system upgrades.
Once the additional elements required by interoperable systems become available, the systems that have incorporated the specification will be able to quickly transition to interoperability. The key additional elements are outlined below.”
____________________________________
The document then goes on to cite SNOMED CT, HL7 V2.x and provider and patient identification.
I must say it takes some special form of arrogance to publish a set of specifications such as this without any reference to, or suggestion of, even the simplest of trial implementations, or ‘proof of concept and viability’, or any of the tools that are obviously required to make any sense or use of the material.
I am sure any system provider offered this specification would say: “Where in the world is something of this structure and complexity working and how much are you going to pay me to be your trial horse?”
Comments such as “NEHTA anticipates that, in the first instance, the health community will review the GP and Specialist/Critical Care Referral Content Specification to become familiar with the content and intention of the specification, and plan to implement elements of the specification where possible within planned system upgrades.” provide no assurance any of this is going anywhere in the foreseeable future – and leads to the inevitable question “Why should I spend anything on all this until it is clear that others are?”.
The other obvious problem is that NEHTA says that one does not need to do a comprehensive implementation of this specification but provides no roadmap to guide development and implementation priorities. Unless this is provided this looks like it’s pretty much an 'all or none' in terms of what is needed to begin developing system specifications. And the “all” is a huge project I would suggest, especially as the specification seems to only exist as an untested MS Word document at present!
The last major issue is that nowhere in the documentation is there any mention of how interoperation, if ever attempted, will be certified and provide a robust guarantee of accuracy, reliability, future maintenance and safety. If you offer a specification of this nature for use you take on the obligation to maintain and certify compliance with the specifications that you produce in perpetuity. Plans in this area simply do not exist as far as I can tell.
Slipping back to reality for a moment, the facts are these:
1. A national HealthConnect project, as originally envisaged, seems to have a very low probability of actually ever being implemented, even though NEHTA says it is still being worked on. The most obvious reason for this is that the costs of such a project (almost certainly billions of dollars) are not likely to easily be provided by Government – despite a compelling business case to make major investments in the e-Health space.
2. The world has moved on to more pragmatic international standards with experts and implementers on both sides of the Atlantic seeking simpler and more practical implementable approaches for deployment of interoperable systems. In the US the Continuity of Care Document (CCD) is emerging (deploying features of HL7, CDA R2 and ASTM CCR) as a credible standard and in the UK work has been undertaken to reduce the information content on the NHS Spine down to the minimum possible.
3. Without a guarantee of major investment in these specifications no vendor will invest to develop compliance. Attempts at mandating such specifications are likewise doomed as large vendors will simply say 'you set up the certification mechanisms so compliance can be verified and you pay us all our costs at time and material rates and we will develop what you require!” Meanwhile, small vendors will probably be put out of business if they attempt to address the complexity inherent in the specifications.
4. Unless the specification is implemented as a whole how are partially compliant systems to ‘understand’ what they are being sent? There are also versioning and maintenance issues that will emerge over time that are not addressed as best I can see. What is likely to happen as new versions of this specification are developed or new terminology is implemented. All of a sudden interoperation between old and new versions will become much more problematic. OpenEHR and its predecessor designs have devoted vast effort to addressing such matters. It is not clear the same is true with this work.
It seems clear that as of now, NEHTA would be far better off working with HL7 to spend whatever limited resources are available to assist with and influence the CCD and make sure it is suitable for Australia rather than continuing with what is an ill-considered, go it alone, and now past its time, local initiative. That way, more local skills in support of a global standard and its implementation would be developed in Australia. This in turn would enable Australia to maintain a place at the 'top table' of standards developers, and ensure that it can draw upon various sources of implementation capabilities and resources internationally.
Unless NEHTA is prepared to fund a range of genuine ‘proof of concept’ implementations of its specifications (to confirm their functionality, utility, viability and technical correctness) this is all going to be a waste of time and money. Even if NEHTA does decide to take that path the likelihood of eventual adoption by the Australian Health IT community would have to be rated as unlikely at best.
David.
Monday, March 05, 2007
Why Should Commonwealth e-Health Executives be having Sleepless Nights?
NEHTA gave a presentation at the 9th Annual AFR Health Congress last week. This presentation confirms my worst fears. From the presentation it is now clear that fantasy and wishful thinking have replaced any rationality that may have once been evident.
I am now able to confidently declare the NEHTA experiment to be a dangerous, destructive (of many committed professionals in the area) and expensive failure, and I am confident it will soon become a 'career limiting' blot on the resumes of many of those involved.
It cannot be too long before the Minister is forced to intervene and try and rescue some of the worthwhile cargo from the sinking ship. How can I be sure? Let me provide the evidence.
Let's start with the title of the presentation “Accelerating e-Health in Australia”. This is hardly true – we are told in the presentation that the time frame for benefits realisation is 10 years and that current implementation plans for the most basic of services will take at least 3-4 years from now.
NEHTA claims to be managing four major projects. Let us consider each in turn
1. Benefits – Seeking to identify the greatest benefits for least cost, in the shortest time, with least risk
Great words but from where will the benefits come?
We are told the benefits will come from (presumed enhancements in):
“Safety –reduced incidence & severity of injury
Effectiveness –avoiding under-use, misuse & over-use
Patient-centeredness -supports continuity of care & patient self-management
Timelines –reducing queues, overcrowding, harmful delays
Efficiency –avoiding waste in equipment, supplies, resources
Equity –in location, socioeconomic status, ethnicity & gender”
What we are not told is ‘the how’. What systems, doing what, used by whom, paid for by whom, with what functionality and so on will yield this bounty?
The benefits are said to be coming from improvements in pharmacy, hospital and general practice processes, messaging efficiency and clinical decision support. How much more generic could one be. Of course if you put quality systems in to support these activities there will probably be benefits.
Work like this was done over five years ago in the US, UK and Canada and it was done better and provided much more detail regarding the systems required, the dependencies and the scale of investment required.
Furthermore the brightly coloured graphs provided are completely meaningless as they lack any scales, values or axes. I would suggest that benefits claimed without any quantification (or even estimates) are hardly real believable benefits. Where, one asks, is the information to support these slides – secret I suppose yet again – or does it actually exist?
Without this information what we have is a claim for benefits derived from systems we don't presently have and at present do not seem to have any plans (or funds) to purchase. It is fantastic – in the true sense of that word.
The two reasons to undertake benefits studies are to justify investment in Health IT and to assist in the management of benefits realisation during system implementation. What NEHTA provides is wholly inadequate to either task. Without much more detail one is left with the distinct impression no detail exists when it is clear a compelling case for investment can be made and should be made but this must be backed up by substance and free of the motherhood as provided here.
2. Identifiers -Uniquely identifying individuals and healthcare providers across Australia
This project has been overtaken by events. With the decision to implement the Human Services Access Card in April 2006, there should have been an immediate review by NEHTA of the plans earlier (February 2006) for identification management systems, to understand how the Access Card proposal could be best melded with the need for individual identification in the e-health environment before too much time and money were wasted.
This has not happened and any relationship between the two projects is disavowed by NEHTA. This is just silly! The facts are:
(a) The Access Card is intended to identify Health Sector Clients for Medicare Benefits and NEHTA is planning to use Medicare ID data for its Identifier.
(b) Both Projects are allocating citizens an ID number and establishing a data-base of basic demographic information.
(c) The NEHTA identifier will be allocated to citizens without their knowledge or consent and if errors occur the citizen will not have access to correct and view the information held.
(d) The NEHTA identifier is likely to be both less 'robust' and more potentially privacy invasive due to its covert existence.
I suspect NEHTA has been given some money and really wants to spend it – and that the ultimate casualty will be a very angry public when it is realised how they are all essentially being secretly numbered while at the same time having to obtain an access card. Again this seems to me to be 'career limiting' for the responsible bureaucrats if not remedied.
3. Terminologies -Exchanging clinical information electronically, using a common language with consistent terms, descriptions and formats.
This is important work but it is not being delivered at the pace NEHTA promised. It is clear the Australian Medicines Terminology extension of SNOMED CT (the national clinical terminology) is significantly delayed (it was promised for January 2007) and the work released on pathology terminology is, by NEHTA's own admission, not ready for implementation.
Without attributing any blame it is also clear that negotiations to set up the international Standards Development Organisation to manage SNOMED CT is also taking longer than expected. (It was meant to be done late in 2006).
4. Shared EHR (SEHR) -Designing a national system of shared electronic health records for authorised practitioners and consumers.
Work in this area would seem to have slowed to a dawdle with only a two page statement of intent issued in the last twelve months (in August 2006). I suspect those responsible have recognised that a national SEHR is much bigger and more complex than they ever envisaged when they were given the abandoned carcass of the HealthConnect project to resurrect in late 2004.
It is worth noting that the time frame for the review of SEHR Standards was twelve to eighteen months after the development of the original report on February 2006. Since that time very little progress seems to have been made with EN13606 (which is still not approved) and NEHTA has apparently declined the opportunity to further develop HL7 V2.x messaging templates as an interim clinical content transfer approach. Meanwhile there has been significant progress on the HL7 Services front and on CDA R2, CCR and CCD making much of the work done in late 2005 for the report obsolete and urgently in need of re-assessment.
5. The fifth project, which is only partially mentioned in the presentation is the development of Secure Messaging for the Health System and the associated Clinical Data Standards for a number of key messages (Discharge Summaries, Referrals etc).
Here we have the secure message providers (HealthLink, Medical Objects, Argus Connect, Promedicus.net, and others) essentially being forced into going their own ways – based on HL7 V2.x or PIT – and the Clinical Data Standards Project continuing on with work based on HealthConnect’s requirements of 2004/5 whilst essentially ignoring the now internationally standardised alternatives for practical health information sharing. It just gets sillier and more wasteful by the month.
What is to be done?
I think the first thing that is needed are the facts. For that reason, as I have suggested previously, I believe we need a professionally conducted enquiry into e-Health for the last decade to get out in the open all the secret reports and make transparent just what has gone well and what has gone badly. The enquiry should also include a thorough audit of the status quo in regards to NEHTA's activities, work-plans, project management structure(s), budgeting and financial controls. This is particularly important in order to see behind the corporate veil which NEHTA has constructed that enables it to avoid being subjected to the rigours of public accountability.
This enquiry would be like the independent enquires conducted in the UK by the Audit Office or in the US by the Government Accountability Office. It would be hard to argue that such a review is not warranted – even on the basis of the obvious facts that the initial vision of 2000/2001 has not been anywhere near delivered some six years later and to ask why.
Another reason an enquiry is needed is that I would argue we have never tried a real model of an AHIC (clinician and expert led) governing a technical execution arm. This is what I took the Boston Consulting Group report as aiming to set up. What happened is that the Government set up the technology component with largely only technology leadership and then moved it away from direct DoHA control and placed control with a non-expert (in Health IT) board.
To show how far implementation has slipped one only has to return to the April 2004 Boston Consulting Group Report. Three years following the report it was intended that:
“ Connectivity building blocks largely in place
- 'Critical mass' of new interoperable clinical and administrative systems
- Key standards agreed and implemented by authoritative body
- Significant broad band/required infrastructure roll-out across country
- High-system users aware of consent issues and electronic benefits
- Significant numbers of providers have experience of clinical messaging and order entry applications
- Expanded information available for research, policy purposes and administrative uses.”
How close are we now to this happy state? Look closely at what was recommended and compare with what we presently have.
Source: BCG April 2004.
It is only when armed with independently acquired facts that a really rational and workable forward plan can be developed.
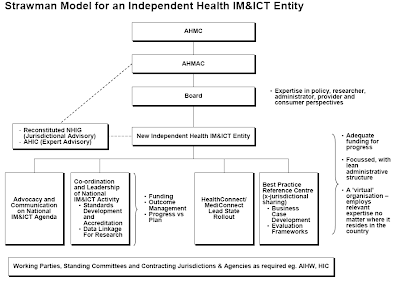
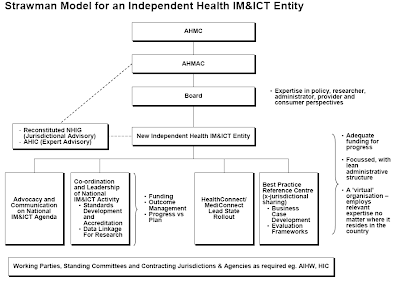
For what its worth I believe that essentially the technologically driven 'tail' needs to stop wagging the health sector 'dog'. If the revised Australian Health Information Council (AHIC) had executive authority, a relevant mix of Health and Health IT experts and appropriate funds, it would be the ideal entity to take direct control of the NEHTA agenda and work plan. As this does not seem to be the case an alternative approach is required.
As I see it, the problem is that there really needs to be a holistic strategic and low level integrated approach i.e. all the aspects from identifying the problems, finding approaches and solutions, then doing the actual work [differentiating what should be done by the market and by Government(s)] in a co-ordinated way at the technical, standards and strategic levels.
Having a non-strategic 'tech shop', which operates in a strategic vacuum, and which claims strategic responsibility for Australian E-Health is a real problem - they (the Council of Australian Governments) have created a strategically 'headless chook' and we are now seeing the results.
So NEHTA has become the answer to a question that was not properly framed by the Boston Consulting Group - and this has led, combined with the dismemberment of AHIC, to the dysfunction we now see.
The reason we have gone down this path is that the business case, which should have been acceptable to Government to initiate a reasonable level of investment, was never done (as it was in the US, UK and Canada) and so, without any real investment co-ordination and scale, nothing has happened. And nothing will happen until that changes and this joke of an effort which masquerades as a business case from NEHTA (see the two colour slides) is redone to really get us there. There is good evidence available and this effort does not exploit it at all.
NEHTA does not see the gap between what it is doing and the need to have a real, achievable and immediate impact on health services (which is, I believe, huge).
We need a fully funded strategic e-Health entity which has the role of driving NEHTA down a more health sector focussed role and setting priorities for the whole sector - with a mix of vendor and home developed solutions and an openness to working with industry, academia, clinicians, and others.
It might be possible to add to NEHTA a strategy unit and a decent health sector liaison unit and change the CEO to someone more fitted to the role. The present leadership have shown an absence of strategic nous and health sector understanding and should only continue in operational delivery rather than strategic planning roles.
We also need to get real political accountability back - so heat can be felt and reacted to for the betterment of all! NEHTA really needs to be back under normal public sector management and accountability.
At HIMMS 07 (a few days ago) we had NEHTA deliver a presentation entitled “Successful E - Health Transitions: Australia's E- Health Initiatives”. Given what NEHTA has failed to deliver over the last three years or so, I would hate to know what failure looked like if this is success!
A major strategic change is needed, based on real independent evidence of what is working and what is not, and it can't come soon enough. The bureaucrats who are fond of their jobs really need to get a reality check, and initiate major change of the sort I outline, or suffer a pretty nasty fate once the Minister realises just how badly things have really gone, how many lives have been damaged or worse, and how much money has been wasted.
David.
I am now able to confidently declare the NEHTA experiment to be a dangerous, destructive (of many committed professionals in the area) and expensive failure, and I am confident it will soon become a 'career limiting' blot on the resumes of many of those involved.
It cannot be too long before the Minister is forced to intervene and try and rescue some of the worthwhile cargo from the sinking ship. How can I be sure? Let me provide the evidence.
Let's start with the title of the presentation “Accelerating e-Health in Australia”. This is hardly true – we are told in the presentation that the time frame for benefits realisation is 10 years and that current implementation plans for the most basic of services will take at least 3-4 years from now.
NEHTA claims to be managing four major projects. Let us consider each in turn
1. Benefits – Seeking to identify the greatest benefits for least cost, in the shortest time, with least risk
Great words but from where will the benefits come?
We are told the benefits will come from (presumed enhancements in):
“Safety –reduced incidence & severity of injury
Effectiveness –avoiding under-use, misuse & over-use
Patient-centeredness -supports continuity of care & patient self-management
Timelines –reducing queues, overcrowding, harmful delays
Efficiency –avoiding waste in equipment, supplies, resources
Equity –in location, socioeconomic status, ethnicity & gender”
What we are not told is ‘the how’. What systems, doing what, used by whom, paid for by whom, with what functionality and so on will yield this bounty?
The benefits are said to be coming from improvements in pharmacy, hospital and general practice processes, messaging efficiency and clinical decision support. How much more generic could one be. Of course if you put quality systems in to support these activities there will probably be benefits.
Work like this was done over five years ago in the US, UK and Canada and it was done better and provided much more detail regarding the systems required, the dependencies and the scale of investment required.
Furthermore the brightly coloured graphs provided are completely meaningless as they lack any scales, values or axes. I would suggest that benefits claimed without any quantification (or even estimates) are hardly real believable benefits. Where, one asks, is the information to support these slides – secret I suppose yet again – or does it actually exist?
Without this information what we have is a claim for benefits derived from systems we don't presently have and at present do not seem to have any plans (or funds) to purchase. It is fantastic – in the true sense of that word.
The two reasons to undertake benefits studies are to justify investment in Health IT and to assist in the management of benefits realisation during system implementation. What NEHTA provides is wholly inadequate to either task. Without much more detail one is left with the distinct impression no detail exists when it is clear a compelling case for investment can be made and should be made but this must be backed up by substance and free of the motherhood as provided here.
2. Identifiers -Uniquely identifying individuals and healthcare providers across Australia
This project has been overtaken by events. With the decision to implement the Human Services Access Card in April 2006, there should have been an immediate review by NEHTA of the plans earlier (February 2006) for identification management systems, to understand how the Access Card proposal could be best melded with the need for individual identification in the e-health environment before too much time and money were wasted.
This has not happened and any relationship between the two projects is disavowed by NEHTA. This is just silly! The facts are:
(a) The Access Card is intended to identify Health Sector Clients for Medicare Benefits and NEHTA is planning to use Medicare ID data for its Identifier.
(b) Both Projects are allocating citizens an ID number and establishing a data-base of basic demographic information.
(c) The NEHTA identifier will be allocated to citizens without their knowledge or consent and if errors occur the citizen will not have access to correct and view the information held.
(d) The NEHTA identifier is likely to be both less 'robust' and more potentially privacy invasive due to its covert existence.
I suspect NEHTA has been given some money and really wants to spend it – and that the ultimate casualty will be a very angry public when it is realised how they are all essentially being secretly numbered while at the same time having to obtain an access card. Again this seems to me to be 'career limiting' for the responsible bureaucrats if not remedied.
3. Terminologies -Exchanging clinical information electronically, using a common language with consistent terms, descriptions and formats.
This is important work but it is not being delivered at the pace NEHTA promised. It is clear the Australian Medicines Terminology extension of SNOMED CT (the national clinical terminology) is significantly delayed (it was promised for January 2007) and the work released on pathology terminology is, by NEHTA's own admission, not ready for implementation.
Without attributing any blame it is also clear that negotiations to set up the international Standards Development Organisation to manage SNOMED CT is also taking longer than expected. (It was meant to be done late in 2006).
4. Shared EHR (SEHR) -Designing a national system of shared electronic health records for authorised practitioners and consumers.
Work in this area would seem to have slowed to a dawdle with only a two page statement of intent issued in the last twelve months (in August 2006). I suspect those responsible have recognised that a national SEHR is much bigger and more complex than they ever envisaged when they were given the abandoned carcass of the HealthConnect project to resurrect in late 2004.
It is worth noting that the time frame for the review of SEHR Standards was twelve to eighteen months after the development of the original report on February 2006. Since that time very little progress seems to have been made with EN13606 (which is still not approved) and NEHTA has apparently declined the opportunity to further develop HL7 V2.x messaging templates as an interim clinical content transfer approach. Meanwhile there has been significant progress on the HL7 Services front and on CDA R2, CCR and CCD making much of the work done in late 2005 for the report obsolete and urgently in need of re-assessment.
5. The fifth project, which is only partially mentioned in the presentation is the development of Secure Messaging for the Health System and the associated Clinical Data Standards for a number of key messages (Discharge Summaries, Referrals etc).
Here we have the secure message providers (HealthLink, Medical Objects, Argus Connect, Promedicus.net, and others) essentially being forced into going their own ways – based on HL7 V2.x or PIT – and the Clinical Data Standards Project continuing on with work based on HealthConnect’s requirements of 2004/5 whilst essentially ignoring the now internationally standardised alternatives for practical health information sharing. It just gets sillier and more wasteful by the month.
What is to be done?
I think the first thing that is needed are the facts. For that reason, as I have suggested previously, I believe we need a professionally conducted enquiry into e-Health for the last decade to get out in the open all the secret reports and make transparent just what has gone well and what has gone badly. The enquiry should also include a thorough audit of the status quo in regards to NEHTA's activities, work-plans, project management structure(s), budgeting and financial controls. This is particularly important in order to see behind the corporate veil which NEHTA has constructed that enables it to avoid being subjected to the rigours of public accountability.
This enquiry would be like the independent enquires conducted in the UK by the Audit Office or in the US by the Government Accountability Office. It would be hard to argue that such a review is not warranted – even on the basis of the obvious facts that the initial vision of 2000/2001 has not been anywhere near delivered some six years later and to ask why.
Another reason an enquiry is needed is that I would argue we have never tried a real model of an AHIC (clinician and expert led) governing a technical execution arm. This is what I took the Boston Consulting Group report as aiming to set up. What happened is that the Government set up the technology component with largely only technology leadership and then moved it away from direct DoHA control and placed control with a non-expert (in Health IT) board.
To show how far implementation has slipped one only has to return to the April 2004 Boston Consulting Group Report. Three years following the report it was intended that:
“ Connectivity building blocks largely in place
- 'Critical mass' of new interoperable clinical and administrative systems
- Key standards agreed and implemented by authoritative body
- Significant broad band/required infrastructure roll-out across country
- High-system users aware of consent issues and electronic benefits
- Significant numbers of providers have experience of clinical messaging and order entry applications
- Expanded information available for research, policy purposes and administrative uses.”
How close are we now to this happy state? Look closely at what was recommended and compare with what we presently have.
Source: BCG April 2004.
It is only when armed with independently acquired facts that a really rational and workable forward plan can be developed.
For what its worth I believe that essentially the technologically driven 'tail' needs to stop wagging the health sector 'dog'. If the revised Australian Health Information Council (AHIC) had executive authority, a relevant mix of Health and Health IT experts and appropriate funds, it would be the ideal entity to take direct control of the NEHTA agenda and work plan. As this does not seem to be the case an alternative approach is required.
As I see it, the problem is that there really needs to be a holistic strategic and low level integrated approach i.e. all the aspects from identifying the problems, finding approaches and solutions, then doing the actual work [differentiating what should be done by the market and by Government(s)] in a co-ordinated way at the technical, standards and strategic levels.
Having a non-strategic 'tech shop', which operates in a strategic vacuum, and which claims strategic responsibility for Australian E-Health is a real problem - they (the Council of Australian Governments) have created a strategically 'headless chook' and we are now seeing the results.
So NEHTA has become the answer to a question that was not properly framed by the Boston Consulting Group - and this has led, combined with the dismemberment of AHIC, to the dysfunction we now see.
The reason we have gone down this path is that the business case, which should have been acceptable to Government to initiate a reasonable level of investment, was never done (as it was in the US, UK and Canada) and so, without any real investment co-ordination and scale, nothing has happened. And nothing will happen until that changes and this joke of an effort which masquerades as a business case from NEHTA (see the two colour slides) is redone to really get us there. There is good evidence available and this effort does not exploit it at all.
NEHTA does not see the gap between what it is doing and the need to have a real, achievable and immediate impact on health services (which is, I believe, huge).
We need a fully funded strategic e-Health entity which has the role of driving NEHTA down a more health sector focussed role and setting priorities for the whole sector - with a mix of vendor and home developed solutions and an openness to working with industry, academia, clinicians, and others.
It might be possible to add to NEHTA a strategy unit and a decent health sector liaison unit and change the CEO to someone more fitted to the role. The present leadership have shown an absence of strategic nous and health sector understanding and should only continue in operational delivery rather than strategic planning roles.
We also need to get real political accountability back - so heat can be felt and reacted to for the betterment of all! NEHTA really needs to be back under normal public sector management and accountability.
At HIMMS 07 (a few days ago) we had NEHTA deliver a presentation entitled “Successful E - Health Transitions: Australia's E- Health Initiatives”. Given what NEHTA has failed to deliver over the last three years or so, I would hate to know what failure looked like if this is success!
A major strategic change is needed, based on real independent evidence of what is working and what is not, and it can't come soon enough. The bureaucrats who are fond of their jobs really need to get a reality check, and initiate major change of the sort I outline, or suffer a pretty nasty fate once the Minister realises just how badly things have really gone, how many lives have been damaged or worse, and how much money has been wasted.
David.
Sunday, March 04, 2007
An Invaluable Reference on Health IT Value
Just a very short post to make sure everyone is aware of this invaluable site.
It is titled:
The case for IT in healthcare – supporting the patient safety agenda
It contains links and summaries of a large number of reports that have shown a clear case for using IT in healthcare to bring safety benefits for patients.
This is the case we should be making to the Australian Government.
The URL is:
http://www.connectingforhealth.nhs.uk/about/case/the-case-for-it-in-healthcare
Enjoy browsing and use the material to convince others of the importance and value of pressing on with Health IT programs and initiatives.
While citing this site it occurs to me there are other invaluable sites that are well worth a browse.
My special favourites are:
For the USA.
http://www.ihealthbeat.org/
http://healthdatamanagement.com/
http://www.informatics-review.com/
http://www.govhealthit.com/
http://www.healthcareitnews.com/
For the UK.
http://www.informatics.nhs.uk/
http://www.e-health-insider.com/
And in Australia
http://australianit.news.com.au/topics/0,7202,news_ehealth_law,00.html
http://www.pulsemagazine.com.au/
For a link to many Health IT Blogs – this site is useful
http://www.hitsphere.com/
Enjoy browsing them all.
David.
It is titled:
The case for IT in healthcare – supporting the patient safety agenda
It contains links and summaries of a large number of reports that have shown a clear case for using IT in healthcare to bring safety benefits for patients.
This is the case we should be making to the Australian Government.
The URL is:
http://www.connectingforhealth.nhs.uk/about/case/the-case-for-it-in-healthcare
Enjoy browsing and use the material to convince others of the importance and value of pressing on with Health IT programs and initiatives.
While citing this site it occurs to me there are other invaluable sites that are well worth a browse.
My special favourites are:
For the USA.
http://www.ihealthbeat.org/
http://healthdatamanagement.com/
http://www.informatics-review.com/
http://www.govhealthit.com/
http://www.healthcareitnews.com/
For the UK.
http://www.informatics.nhs.uk/
http://www.e-health-insider.com/
And in Australia
http://australianit.news.com.au/topics/0,7202,news_ehealth_law,00.html
http://www.pulsemagazine.com.au/
For a link to many Health IT Blogs – this site is useful
http://www.hitsphere.com/
Enjoy browsing them all.
David.
AusHealthIT Turns One!
Well the blog is one year old on March 5, 2007. It now has one hundred and thirty eight entries and a regular readership that exceeds one hundred and fifty different individuals each time a new article is added.
The current top 10 most read articles are as follows:
1. Personal Health Information Privacy – The Elephant in the Room
2. Archetypically Stupid!
3. Electronic Prescribing – What is Needed to Move Forward?
4. NEHTA’s Annual Report – What We are Not Being Told.
5. Privacy Issues Related to the Proposed Access Card.
6. E-Mail Security and Clinical Practice.
7. E-Prescribing in Australia – Is there a New Plan?
8. How Did iSoft Get into So Much Trouble?
9. Clinical Research Information Now More Freely Available on the Internet.
10. AusHealthIT's First Guest Blogger Article.
Amazingly the different pages on the blog have now been viewed 13,333 times since I worked out how to set up a site counter in May, 2006.
The steady growth in feed subscribers has been encouraging and suggests that at least the blog is of interest and slightly controversial rather than being a total bore!
Feed Subscribers

What is there to learn from all this regarding the current state of and planned directions for E-Health in Australia? I take the following from the level of interest and the comments posted.
1. The topic of Health IT (e-health) is of interest to many more people than would initially be thought.
2. The topics of interest are – with a few exceptions – centred around the need for better policy in the area.
3. The themes of the blog in suggesting the need for a substantive National E-Health Strategy, Business Case and Implementation Plan and clarity around the importance of Health IT in the areas of patient safety and quality of care are supported.
4. The need to have sorted out a plan and then to ‘get on with it’ using proven and known technologies is totally un-controversial. There is widespread amazement in the E-Health community that the opportunity cost of doing nothing in the e-Health space is unrecognised. It is costing the community dearly in both lives and dollars.
5. Frustration with the lack of strategic clarity in the e-Health space is forcing development and implementation activity which is to be welcomed but which could be so much more effective and valuable if undertaken in a supportive, rational and co-ordinated framework.
6. There is widespread disappointment and frustration that NEHTA has focussed too much on the “E” and not enough on the “Health” leaving its efforts being seen as largely irrelevant to the Health Sector in general and increasingly the E-Health Community in particular. It is very important for NEHTA to be successful for E-Health in Australia to prosper and right now it does not seem to be heading in the right direction or listening to the E-Health Community very effectively.
I sense change is coming in this election year and also that Year 2 will be a very interesting one!
I would love comments on the above.
David.
The current top 10 most read articles are as follows:
1. Personal Health Information Privacy – The Elephant in the Room
2. Archetypically Stupid!
3. Electronic Prescribing – What is Needed to Move Forward?
4. NEHTA’s Annual Report – What We are Not Being Told.
5. Privacy Issues Related to the Proposed Access Card.
6. E-Mail Security and Clinical Practice.
7. E-Prescribing in Australia – Is there a New Plan?
8. How Did iSoft Get into So Much Trouble?
9. Clinical Research Information Now More Freely Available on the Internet.
10. AusHealthIT's First Guest Blogger Article.
Amazingly the different pages on the blog have now been viewed 13,333 times since I worked out how to set up a site counter in May, 2006.
The steady growth in feed subscribers has been encouraging and suggests that at least the blog is of interest and slightly controversial rather than being a total bore!
Feed Subscribers

What is there to learn from all this regarding the current state of and planned directions for E-Health in Australia? I take the following from the level of interest and the comments posted.
1. The topic of Health IT (e-health) is of interest to many more people than would initially be thought.
2. The topics of interest are – with a few exceptions – centred around the need for better policy in the area.
3. The themes of the blog in suggesting the need for a substantive National E-Health Strategy, Business Case and Implementation Plan and clarity around the importance of Health IT in the areas of patient safety and quality of care are supported.
4. The need to have sorted out a plan and then to ‘get on with it’ using proven and known technologies is totally un-controversial. There is widespread amazement in the E-Health community that the opportunity cost of doing nothing in the e-Health space is unrecognised. It is costing the community dearly in both lives and dollars.
5. Frustration with the lack of strategic clarity in the e-Health space is forcing development and implementation activity which is to be welcomed but which could be so much more effective and valuable if undertaken in a supportive, rational and co-ordinated framework.
6. There is widespread disappointment and frustration that NEHTA has focussed too much on the “E” and not enough on the “Health” leaving its efforts being seen as largely irrelevant to the Health Sector in general and increasingly the E-Health Community in particular. It is very important for NEHTA to be successful for E-Health in Australia to prosper and right now it does not seem to be heading in the right direction or listening to the E-Health Community very effectively.
I sense change is coming in this election year and also that Year 2 will be a very interesting one!
I would love comments on the above.
David.
Thursday, March 01, 2007
HL7, Seemingly Moving Ahead as Australia Languishes.
Over the last few months there has been a steady stream of announcements and releases from HL7 that, taken together, must be seen as encouraging for the steady improvement in the level of standardisation and interoperation that is possible in implementation of e-Health.
These major announcements have (selectively quoting from the press releases) included:
1. On January 22, 2007 Health Level Seven (HL7) today announced four major milestones toward harmonization of interoperability standards as a result of the HL7 Working Group meeting held January 8 – 13, 2007 in San Diego, CA. HL7’s four key accomplishments include the following:
• HL7 collaboration with the Object Management Group (OMG) has resulted in HL7's Services-Oriented Architecture Committee successfully balloting three Draft Standards for Trial Use (DSTUs), two of which are now adopted and part of the Object Management Group's technology adoption process.
• Collaboration between HL7 and ASTM has resulted in the co-development of the Continuity of Care Document (CCD) endorsed by the Healthcare Information Technology Standards Panel (HITSP) and passed HL7 balloting on January 4, 2007.
• HL7 finalized an agreement with the California Health Care Foundation to ballot the EHR-Lab Interoperability and Connectivity Specification (ELINCS) through HL7 as an implementation guide to enable reporting of lab results from laboratory information systems to electronic health records (EHRs) in the outpatient setting.
• HL7 reached out beyond its existing membership, bringing extensive clinical input into the development of the EHR-S Functional Model. The Functional Model is one step closer to becoming an industry standard, and has already proven to be a useful tool for the Certification Commission for Health Information Technology (CCHIT).
2. On February 12, 2007 Health Level Seven (HL7), announced that, with the collaboration of the ASTM International E31 Healthcare Informatics Committee, the Continuity of Care Document (CCD) has passed HL7 balloting and is endorsed by the Healthcare Information Technology Standards Panel (HITSP) as the harmonized format for the exchange of clinical information including patient demographics, medications and allergies.
The CCD is a joint effort of HL7 and ASTM to foster interoperability of clinical data to allow physicians to send electronic medical information to other providers without loss of meaning, which will ultimately improve patient care.
“The collaboration between HL7 and ASTM reflects the integration of two complementary specifications [ASTM’s E2369-05, Continuity of Care Record (CCR), and HL7’s Clinical Document Architecture (CDA)] developed by separate standards development organizations, and demonstrates what can be achieved when patient care is the driving priority,” said Robert Dolin, MD, co-editor of the CCD specification and board member of HL7.
3 On February 21, 2007 Health Level Seven (HL7), announced it has passed the healthcare industry’s first ANSI-approved standard that specifies the functional requirements for an electronic health record system (EHR-S).
The standard outlines important features and functions that should be contained in an EHR system. The standard’s Functional Model contains approximately 1,000 conformance criteria across 130 functions, including medication history, problem lists, orders, clinical decision support, and those supporting privacy and security.
The function list is described from a user perspective and enables consistent expression of EHR system functionality, while the conformance criteria serves as a reference for purchasers of EHR systems and vendors developing EHR software.”
These announcements are all pragmatic and considered incremental steps in the level of e-Health standardisation and all have been either been proven through actual implementation or are provided as Draft Standards for Trial Use – and will only be made full standards once proven. I hope those responsible in Australia are monitoring the progress carefully and planning to take full advantage of the positive outcomes.
All this good news is not to deny that there are still some remaining issues with the HL7 project – most especially with HL7 V3.0. These issues are reviewed and discussed by a fellow blogger at the following URL:
http://hl7-watch.blogspot.com/
Having browsed his work I am sure Professor Smith would be as pleased as I am to see the continuing development of the HL7 V2.x standards while the complexity and wrinkles in Version 3.0 are worked through and a practical and fully usable standard emerges. Version 3.0 has now been over 10 years in the making so one can only hope it won’t be too much longer! There are some serious organisations (like the UK NHS) pinning their hopes on success soon. I also have a sense that NEHTA is developing specifications and standards which may require years in the implementation while from HL7 we are getting some real guidance that could move things along far more quickly.
On a related topic I happened to see a copy of the ISO/TC 215 Health Informatics
Opening Plenary Final Agenda and associated papers for the meeting of March 2007 in Montreal Canada. I have to say that I was surprised just how much of the material that was to be covered was termed to be in a ‘Preliminary” state. It would be good to see rapid progress at this meeting also!
David.
These major announcements have (selectively quoting from the press releases) included:
1. On January 22, 2007 Health Level Seven (HL7) today announced four major milestones toward harmonization of interoperability standards as a result of the HL7 Working Group meeting held January 8 – 13, 2007 in San Diego, CA. HL7’s four key accomplishments include the following:
• HL7 collaboration with the Object Management Group (OMG) has resulted in HL7's Services-Oriented Architecture Committee successfully balloting three Draft Standards for Trial Use (DSTUs), two of which are now adopted and part of the Object Management Group's technology adoption process.
• Collaboration between HL7 and ASTM has resulted in the co-development of the Continuity of Care Document (CCD) endorsed by the Healthcare Information Technology Standards Panel (HITSP) and passed HL7 balloting on January 4, 2007.
• HL7 finalized an agreement with the California Health Care Foundation to ballot the EHR-Lab Interoperability and Connectivity Specification (ELINCS) through HL7 as an implementation guide to enable reporting of lab results from laboratory information systems to electronic health records (EHRs) in the outpatient setting.
• HL7 reached out beyond its existing membership, bringing extensive clinical input into the development of the EHR-S Functional Model. The Functional Model is one step closer to becoming an industry standard, and has already proven to be a useful tool for the Certification Commission for Health Information Technology (CCHIT).
2. On February 12, 2007 Health Level Seven (HL7), announced that, with the collaboration of the ASTM International E31 Healthcare Informatics Committee, the Continuity of Care Document (CCD) has passed HL7 balloting and is endorsed by the Healthcare Information Technology Standards Panel (HITSP) as the harmonized format for the exchange of clinical information including patient demographics, medications and allergies.
The CCD is a joint effort of HL7 and ASTM to foster interoperability of clinical data to allow physicians to send electronic medical information to other providers without loss of meaning, which will ultimately improve patient care.
“The collaboration between HL7 and ASTM reflects the integration of two complementary specifications [ASTM’s E2369-05, Continuity of Care Record (CCR), and HL7’s Clinical Document Architecture (CDA)] developed by separate standards development organizations, and demonstrates what can be achieved when patient care is the driving priority,” said Robert Dolin, MD, co-editor of the CCD specification and board member of HL7.
3 On February 21, 2007 Health Level Seven (HL7), announced it has passed the healthcare industry’s first ANSI-approved standard that specifies the functional requirements for an electronic health record system (EHR-S).
The standard outlines important features and functions that should be contained in an EHR system. The standard’s Functional Model contains approximately 1,000 conformance criteria across 130 functions, including medication history, problem lists, orders, clinical decision support, and those supporting privacy and security.
The function list is described from a user perspective and enables consistent expression of EHR system functionality, while the conformance criteria serves as a reference for purchasers of EHR systems and vendors developing EHR software.”
These announcements are all pragmatic and considered incremental steps in the level of e-Health standardisation and all have been either been proven through actual implementation or are provided as Draft Standards for Trial Use – and will only be made full standards once proven. I hope those responsible in Australia are monitoring the progress carefully and planning to take full advantage of the positive outcomes.
All this good news is not to deny that there are still some remaining issues with the HL7 project – most especially with HL7 V3.0. These issues are reviewed and discussed by a fellow blogger at the following URL:
http://hl7-watch.blogspot.com/
Having browsed his work I am sure Professor Smith would be as pleased as I am to see the continuing development of the HL7 V2.x standards while the complexity and wrinkles in Version 3.0 are worked through and a practical and fully usable standard emerges. Version 3.0 has now been over 10 years in the making so one can only hope it won’t be too much longer! There are some serious organisations (like the UK NHS) pinning their hopes on success soon. I also have a sense that NEHTA is developing specifications and standards which may require years in the implementation while from HL7 we are getting some real guidance that could move things along far more quickly.
On a related topic I happened to see a copy of the ISO/TC 215 Health Informatics
Opening Plenary Final Agenda and associated papers for the meeting of March 2007 in Montreal Canada. I have to say that I was surprised just how much of the material that was to be covered was termed to be in a ‘Preliminary” state. It would be good to see rapid progress at this meeting also!
David.
Tuesday, February 27, 2007
AusHealthIT Flash! February 27, 2007
Guess what?
The Australian Health Information Council (AHIC) has been reformed after some two years as the peak E-Health advisory body for Australia.
What is known so far?
1. The new AHIC has no executive authority or significant funds to disperse. It is purely advisory.
2. It has no more than two people in its membership who could be described as Health IT experts
3. It met some time last week apparently – but somehow the meeting date, time and attendees and topics discussed are a secret!
4. The role of the new committee is ‘Long Term Strategy’.
5. Apparently a communiqué is being drafted by DoHA so the great unwashed can get to know what is going on.
The time has come for all this to become a serious political issue as it is clear the present Government has no intent or capability to change things. Lives are being lost today as ‘long term strategy’ is being toyed with!
For the record www.ahic.org.au is still not operational (or .gov)
As the BBC says on their news website – “More soon”
For those interested my article of the 13 October, 2006 explains what is needed from a new AHIC. I leave it as an exercise for the reader to work out how close we have come in function, transparency and expertise!
Frankly, this is just hopeless. It seems to be secret, not well informed and impotent – just what the health system needs to manage the E-Health domain.
David.
The Australian Health Information Council (AHIC) has been reformed after some two years as the peak E-Health advisory body for Australia.
What is known so far?
1. The new AHIC has no executive authority or significant funds to disperse. It is purely advisory.
2. It has no more than two people in its membership who could be described as Health IT experts
3. It met some time last week apparently – but somehow the meeting date, time and attendees and topics discussed are a secret!
4. The role of the new committee is ‘Long Term Strategy’.
5. Apparently a communiqué is being drafted by DoHA so the great unwashed can get to know what is going on.
The time has come for all this to become a serious political issue as it is clear the present Government has no intent or capability to change things. Lives are being lost today as ‘long term strategy’ is being toyed with!
For the record www.ahic.org.au is still not operational (or .gov)
As the BBC says on their news website – “More soon”
For those interested my article of the 13 October, 2006 explains what is needed from a new AHIC. I leave it as an exercise for the reader to work out how close we have come in function, transparency and expertise!
Frankly, this is just hopeless. It seems to be secret, not well informed and impotent – just what the health system needs to manage the E-Health domain
David.
Sunday, February 25, 2007
Its Really Nice to Know You Were Right!
Well the chickens have come home to roost! Even allowing for a fifty percent margin of error E-Health in Australia is only moving forward very slowly and is certainly not progressing with the urgency hoped for by Minister Abbott!
The goal was set in June 2005. A report, from that time, of the Minister’s remarks is as follows:
See http://www.computerworld.com.au/index.php?id=1737192765&eid=-6787 for the full article.
“E-health put on notice
Health Minister Tony Abbott has put federal health IT bureaucrats on notice saying he expects tangible results within a year, specifically functioning electronic health records and accompanying smartcard system - or heads would start to roll.
"I am sick of trials and studies and working groups," Abbott said.
"I want patients to see a difference in 12 months. If patients do not see a difference, we will have failed," Abbot said, adding he was not prepared to be "held hostage" by a never-ending chase for the latest and greatest IT solutions.
"For too long we have tried to achieve too much. The best is the enemy of the good."
Asked whether he was prepared to force Australia's eight state and territory health systems to adopt federal health IT standards by linking their funding to outcomes stipulated by Canberra, Abbott said that state health ministers were as frustrated as he was with the seeming lack of progress and that there was no need for [force].
He was far less generous to federal IT practitioners.
"Maybe I should make some federal public servants' pay dependent on outcomes," Abbott said.
A spokesman for Abbott insisted the comment was made in jest, but that public servants were still required to deliver within the 12-month window. "Look, it can't go on forever," the spokesperson said.
As for whether the government is considering a "central database", the spokesperson said Abbott meant "you have to put the information somewhere."
And directly from a Speech in August 2005:
“E-health is a high priority for the Howard Government. It was the subject of my first scripted speech as health minister. The subsequent 20 months have seen solid progress: the establishment of the National E-Health Transition Authority; the launch of a Medicare smart card in Tasmania; the beginnings of HealthConnect in South Australia; and the substantial completion of many of the trials necessary to enable the widespread effective use of IT in health care.”
Think for one moment where these are now? Medicare Smartcard canned, HealthConnect on the deep backburner, and NEHTA now talking of a future taking many years before some real outcomes will be seen.
It seems pretty clear that for all the words – essentially zilch has really happened that has made any difference to the quality and safety of our healthcare system.
A good measure of the actual progress comes from the Department of Health and Ageing (DoHA) 2005/06 Annual Report (p133) where we learn e-Health initiatives have now impacted on10,444 consumers (of the possible 20 million or so).
The E-health targets that the report cites in the section reviewing last years performance, and which it claims have been met, are classics in goal post transport, reversal and remodelling. Rather than report on HealthConnect, which by no way could be said to really exist, the performance measures now relate to broadband installation and the establishment of NEHTA (which was largely in 2004/05 anyway). (p139).
On the next page we also discover E-Health was one of the reasons for the Government underspend on Health! (A $7+million underspend against a (very tiny) $50 million budget)
NEHTA and the DoHA bureaucrats must be wondering when the Minister will ask why it is being so slow spending the funds it has been given. (Note this excludes the other $130 million provided by COAG in February 2006 to NEHTA)
It can’t be said the Minister wasn’t warned. Witness the my comments, as reported in July 2005, after Minister Abbott said a EHR system would be operational in 12 months.
http://www.computerworld.com.au/index.php/id;1140691972
“Academic says HealthConnect will not meet Abbott's timeframe
Michael Crawford 07/07/2005 09:56:10
Health Minister Tony Abbott's ambitious plan to have an electronic health record system operational is highly unlikely to meet a 12 month timeframe according to Dr David More, adjunct professor of Health Informatics at the University of Canberra.
Raising serious doubts about the federal government's ability to meet Abbott's strict schedule, Dr More said the only way the deadline can be met is if doctors get a working client system that is linked to HealthConnect up and running within the next few months.
Dr More, who is a Fellow of the Australian College of Health Informatics, said the government should have committed "real money" to an electronic health record system years ago.
"To have HealthConnect operational, doctors need to have a working and usable client on their desks immediately; this client will need to have advanced clinical decision support and use a fully standards-based infrastructure as well as provide for proper management of privacy and data security," More said.
"The task to develop and implement such a client nationally is just too big to be completed within 12 months. HealthConnect has so far been a seven-year project and look how far it is from that outcome today.
"Our medical system is based on a fee for service per item of service, so the incentive is for a doctor to get as many people through the practice as possible to maximize what he bills," he said, adding that the implementation of new technology will slow doctors down.
"Widespread adoption of a new client system will be slow without major financial incentives to make up for the costs and reduced income."
More also said the Australian medical software industry may not have the skills and expertise available to meet the demands of developing and implementing systems for a national electronic health system without a major injection of funds.
"The government needs to get serious about the amount of money it is prepared to spend in order to get such a system actually working," he said. "To try and duplicate the technology doctors already have would not make sense; they need intelligent, networked systems."
Dr More pointed to the UK's e-health program where the government has committed £10 billion ($23.5 billion) over 10 years.
The US has also committed billions to an electronic health record system over the next few years.
"Essentially we are talking megabucks to implement an advanced electronic system and to do it properly," he said.
In the 2005 Federal budget handed down in May, the government made available $20 million over three years for an electronic health record system.”
Given the article is essentially one large quote of my comments and is 18 months old I hope Computerworld won’t mind if I quote the article in full.
What is unarguable is that, while there have been some small steps forward, (I hear of some good things happening in small pockets all around the country) the lack of a coherent national strategy and reasonable funding ensures – as NEHTA now admits – we are still years away from an implemented and successful national approach.
Right now, it’s a hopeless mess that needs fixing. I hope someone is listening.
David.
The goal was set in June 2005. A report, from that time, of the Minister’s remarks is as follows:
See http://www.computerworld.com.au/index.php?id=1737192765&eid=-6787 for the full article.
“E-health put on notice
Health Minister Tony Abbott has put federal health IT bureaucrats on notice saying he expects tangible results within a year, specifically functioning electronic health records and accompanying smartcard system - or heads would start to roll.
"I am sick of trials and studies and working groups," Abbott said.
"I want patients to see a difference in 12 months. If patients do not see a difference, we will have failed," Abbot said, adding he was not prepared to be "held hostage" by a never-ending chase for the latest and greatest IT solutions.
"For too long we have tried to achieve too much. The best is the enemy of the good."
Asked whether he was prepared to force Australia's eight state and territory health systems to adopt federal health IT standards by linking their funding to outcomes stipulated by Canberra, Abbott said that state health ministers were as frustrated as he was with the seeming lack of progress and that there was no need for [force].
He was far less generous to federal IT practitioners.
"Maybe I should make some federal public servants' pay dependent on outcomes," Abbott said.
A spokesman for Abbott insisted the comment was made in jest, but that public servants were still required to deliver within the 12-month window. "Look, it can't go on forever," the spokesperson said.
As for whether the government is considering a "central database", the spokesperson said Abbott meant "you have to put the information somewhere."
And directly from a Speech in August 2005:
“E-health is a high priority for the Howard Government. It was the subject of my first scripted speech as health minister. The subsequent 20 months have seen solid progress: the establishment of the National E-Health Transition Authority; the launch of a Medicare smart card in Tasmania; the beginnings of HealthConnect in South Australia; and the substantial completion of many of the trials necessary to enable the widespread effective use of IT in health care.”
Think for one moment where these are now? Medicare Smartcard canned, HealthConnect on the deep backburner, and NEHTA now talking of a future taking many years before some real outcomes will be seen.
It seems pretty clear that for all the words – essentially zilch has really happened that has made any difference to the quality and safety of our healthcare system.
A good measure of the actual progress comes from the Department of Health and Ageing (DoHA) 2005/06 Annual Report (p133) where we learn e-Health initiatives have now impacted on10,444 consumers (of the possible 20 million or so).
The E-health targets that the report cites in the section reviewing last years performance, and which it claims have been met, are classics in goal post transport, reversal and remodelling. Rather than report on HealthConnect, which by no way could be said to really exist, the performance measures now relate to broadband installation and the establishment of NEHTA (which was largely in 2004/05 anyway). (p139).
On the next page we also discover E-Health was one of the reasons for the Government underspend on Health! (A $7+million underspend against a (very tiny) $50 million budget)
NEHTA and the DoHA bureaucrats must be wondering when the Minister will ask why it is being so slow spending the funds it has been given. (Note this excludes the other $130 million provided by COAG in February 2006 to NEHTA)
It can’t be said the Minister wasn’t warned. Witness the my comments, as reported in July 2005, after Minister Abbott said a EHR system would be operational in 12 months.
http://www.computerworld.com.au/index.php/id;1140691972
“Academic says HealthConnect will not meet Abbott's timeframe
Michael Crawford 07/07/2005 09:56:10
Health Minister Tony Abbott's ambitious plan to have an electronic health record system operational is highly unlikely to meet a 12 month timeframe according to Dr David More, adjunct professor of Health Informatics at the University of Canberra.
Raising serious doubts about the federal government's ability to meet Abbott's strict schedule, Dr More said the only way the deadline can be met is if doctors get a working client system that is linked to HealthConnect up and running within the next few months.
Dr More, who is a Fellow of the Australian College of Health Informatics, said the government should have committed "real money" to an electronic health record system years ago.
"To have HealthConnect operational, doctors need to have a working and usable client on their desks immediately; this client will need to have advanced clinical decision support and use a fully standards-based infrastructure as well as provide for proper management of privacy and data security," More said.
"The task to develop and implement such a client nationally is just too big to be completed within 12 months. HealthConnect has so far been a seven-year project and look how far it is from that outcome today.
"Our medical system is based on a fee for service per item of service, so the incentive is for a doctor to get as many people through the practice as possible to maximize what he bills," he said, adding that the implementation of new technology will slow doctors down.
"Widespread adoption of a new client system will be slow without major financial incentives to make up for the costs and reduced income."
More also said the Australian medical software industry may not have the skills and expertise available to meet the demands of developing and implementing systems for a national electronic health system without a major injection of funds.
"The government needs to get serious about the amount of money it is prepared to spend in order to get such a system actually working," he said. "To try and duplicate the technology doctors already have would not make sense; they need intelligent, networked systems."
Dr More pointed to the UK's e-health program where the government has committed £10 billion ($23.5 billion) over 10 years.
The US has also committed billions to an electronic health record system over the next few years.
"Essentially we are talking megabucks to implement an advanced electronic system and to do it properly," he said.
In the 2005 Federal budget handed down in May, the government made available $20 million over three years for an electronic health record system.”
Given the article is essentially one large quote of my comments and is 18 months old I hope Computerworld won’t mind if I quote the article in full.
What is unarguable is that, while there have been some small steps forward, (I hear of some good things happening in small pockets all around the country) the lack of a coherent national strategy and reasonable funding ensures – as NEHTA now admits – we are still years away from an implemented and successful national approach.
Right now, it’s a hopeless mess that needs fixing. I hope someone is listening.
David.
Subscribe to:
Posts (Atom)